Welcome to our article on knee osteoarthritis, a degenerative joint disease that primarily affects the knee. As we age, our joints may undergo wear and tear, leading to joint degeneration and conditions like knee osteoarthritis. While it is more common in individuals aged 50 and above, there is an emerging trend of younger patients developing this condition, putting them at risk of early onset. Knee osteoarthritis can have a significant impact on an individual’s quality of life, hindering mobility and causing discomfort.
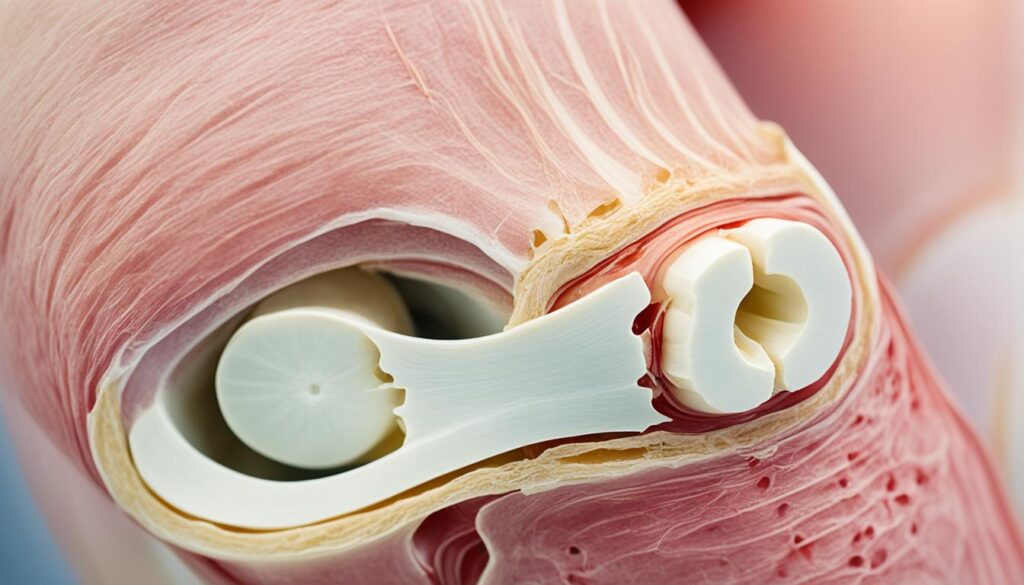
So, how do you recognize the signs of knee osteoarthritis? Pay attention to symptoms such as knee pain, stiffness in the joint, clicking sounds, pain when touching a certain area of the knee, and joint deformities. These symptoms of knee osteoarthritis can vary from person to person but may progressively worsen if left untreated. The image below illustrates the potential joint degeneration that occurs in knee osteoarthritis:
If you suspect you may be experiencing knee osteoarthritis, it is important to seek medical attention for an accurate diagnosis. In the following sections, we will explore the causes of knee osteoarthritis, how to recognize its symptoms, the diagnostic process, available treatment options, and potential consequences if left untreated. Our goal is to provide you with the information you need to understand knee osteoarthritis and make informed decisions about your health.
What Causes Knee Osteoarthritis?
Knee osteoarthritis is a debilitating condition that occurs primarily due to joint wear and tear, age-related degeneration, and various associated factors. The knee joint is susceptible to overuse, making it more prone to osteoarthritis development. This section will explore the key risk factors that contribute to knee osteoarthritis.
Risk Factors for Knee Osteoarthritis
- Previous Knee Injuries: Individuals who have experienced previous knee injuries, such as ligament tears or fractures, are at a higher risk of developing knee osteoarthritis. Injury-related damage to the joint structures can accelerate the degeneration process.
- Unhealthy Diet and Obesity: An unhealthy diet leading to obesity can put excessive stress on the knee joints. The extra weight increases the mechanical load, leading to increased wear and tear on the joint surfaces.
- Underlying Conditions: Certain underlying conditions, such as rheumatoid arthritis or gout, can increase the risk of developing knee osteoarthritis. These conditions contribute to joint inflammation and damage, accelerating the degenerative process.
These risk factors gradually wear away at the joint surface, leading to pain, inflammation, and eventually joint deformities. It is crucial to recognize and address these risk factors to mitigate the development and progression of knee osteoarthritis.
| Risk Factors | Description |
|---|---|
| Previous Knee Injuries | Individuals with a history of knee injuries, such as ligament tears or fractures, are at higher risk. |
| Unhealthy Diet and Obesity | An unhealthy diet leading to obesity increases the mechanical load on the knee joints, accelerating wear and tear. |
| Underlying Conditions | Conditions like rheumatoid arthritis or gout can contribute to joint inflammation and damage, increasing the risk of knee osteoarthritis. |
Recognizing the Symptoms of Knee Osteoarthritis
The symptoms of knee osteoarthritis can vary from person to person, but they often manifest as:
- Knee pain that comes and goes over a period of at least 6 months
- Pain after engaging in activities that put strain on the knee
- Morning stiffness in the knee or stiffness after a period of rest
- A clicking sound in the knee during movement
- Pain when pressing on a specific area of the knee
- Knee deformities, such as bony protrusions
- Swelling of the knee
If left untreated, these symptoms can worsen over time and significantly impact an individual’s daily life. The persistent pain and limitations in mobility can make it challenging to perform essential tasks and enjoy activities. It is crucial to recognize these symptoms and seek medical attention to receive an accurate diagnosis and appropriate treatment.
The Impact of Knee Osteoarthritis Symptoms
The symptoms of knee osteoarthritis can have a profound impact on an individual’s quality of life. The pain and stiffness in the knee can make it difficult to perform simple movements, such as walking, climbing stairs, or getting up from a seated position. The swelling and deformities in the knee joint can further hinder mobility and cause discomfort.
Moreover, the chronic nature of knee osteoarthritis symptoms can lead to frustration, reduced physical activity, and a sedentary lifestyle. This can contribute to weight gain, muscle weakness, and overall decline in health. The emotional and psychological toll of living with knee pain and limitations can also be significant, affecting mental well-being and overall happiness.
Recognizing and addressing these symptoms promptly is crucial to prevent further deterioration, manage pain, and improve overall function and quality of life for individuals with knee osteoarthritis.
A Visual Representation of Knee Osteoarthritis Symptoms
| Symptoms | Description |
|---|---|
| Knee Pain | Persistent pain in the knee joint that lasts for at least 6 months. |
| Knee Stiffness | Difficulty in moving the knee joint, especially in the morning or after a period of rest. |
| Knee Swelling | Visible or palpable swelling around the knee joint. |
| Knee Joint Deformity | Bony protrusions or changes in the shape of the knee joint. |
Understanding the symptoms of knee osteoarthritis and their impact is crucial for early detection, diagnosis, and intervention. Seeking medical advice and exploring appropriate treatment options can aid in managing symptoms, reducing pain, and improving overall comfort and mobility.
Diagnosing Knee Osteoarthritis
A diagnosis of knee osteoarthritis requires a comprehensive approach that combines medical history, physical examination, and imaging tests. When assessing the likelihood of knee osteoarthritis, a doctor may use a basic screening questionnaire to gather relevant information from the patient.
One of the essential tools in diagnosing knee osteoarthritis is a knee x-ray. X-rays provide valuable insight into the condition of the knee joint by detecting narrow spaces within the joint and any abnormalities like enlargement or bone spurs. This imaging test helps confirm the presence of knee osteoarthritis and assess the severity of the condition.
In certain cases, additional imaging tests such as magnetic resonance imaging (MRI) may be necessary. MRIs can provide a more detailed view of the knee joint’s structure, allowing healthcare professionals to rule out other potential causes of joint degeneration and ensure an accurate diagnosis. MRIs are particularly useful for evaluating soft tissues, such as ligaments and cartilage, that may be affected by knee osteoarthritis.
Diagnosing knee osteoarthritis accurately is crucial for determining the most appropriate treatment plan and managing the condition effectively. Through a combination of medical history, physical examination, and imaging tests, healthcare professionals can gain a comprehensive understanding of the condition and provide targeted care.
| Diagnosis Methods | Pros | Cons |
|---|---|---|
| Medical history and physical examination |
|
|
| Knee x-ray |
|
|
| Magnetic Resonance Imaging (MRI) |
|
|
Treatment Options for Knee Osteoarthritis
When it comes to treating knee osteoarthritis, there are several options available. The choice of treatment depends on the individual’s specific situation, taking into consideration factors such as the severity of the condition, the patient’s age, and their overall health. Here are some common treatment options for knee osteoarthritis:
1. Exercise Programs
Exercise is an important component of knee osteoarthritis treatment. It helps improve muscle strength and joint stability, reducing stress on the affected knee. Participating in low-impact exercises such as walking, swimming, or cycling can help relieve pain, increase flexibility, and improve overall joint function.
2. Hyaluronic Acid Injections
Hyaluronic acid injections are a common treatment option for knee osteoarthritis. This procedure involves injecting a gel-like substance into the knee joint to provide lubrication and cushioning, reducing pain and inflammation. Hyaluronic acid injections can improve joint mobility and delay the need for surgery in some cases.
3. Medication
Medication can help manage pain and inflammation associated with knee osteoarthritis. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen can provide relief. In more severe cases, prescription pain medications may be necessary to alleviate discomfort.
4. Physiotherapy
Physiotherapy plays a crucial role in knee osteoarthritis treatment. A physiotherapist can design a personalized exercise program, provide manual therapy techniques, and offer advice on lifestyle modifications to improve pain and mobility. They may also use techniques like heat or cold therapy, ultrasound, or electrical stimulation to relieve symptoms.
5. Arthroscopic Surgery
Arthroscopic surgery may be recommended for individuals with certain knee conditions related to osteoarthritis, such as cartilage tears or loose fragments. This minimally invasive procedure involves making small incisions in the knee and using small instruments to repair or remove damaged tissue. Arthroscopic surgery can help alleviate pain, improve knee function, and delay the need for more invasive procedures like joint replacement.
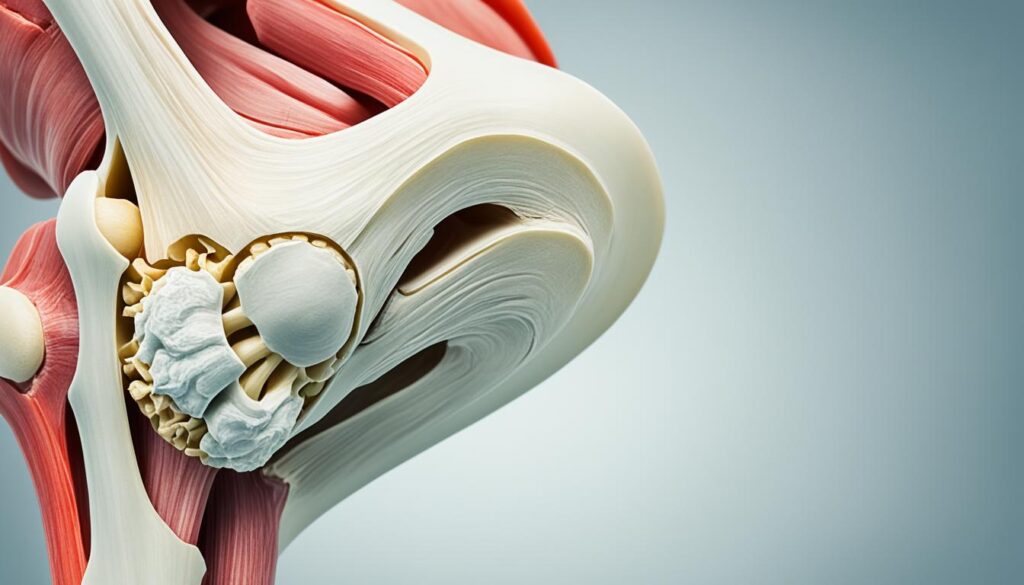
6. Arthroplasty (Joint Replacement Surgery)
In severe cases of knee osteoarthritis where other treatments have not provided relief, joint replacement surgery may be necessary. During this procedure, the damaged parts of the knee joint are replaced with artificial components. Joint replacement surgery can significantly improve joint function, relieve pain, and enhance quality of life for individuals with advanced knee osteoarthritis.
It’s important to note that the choice of treatment depends on various factors, and a healthcare professional should evaluate each patient’s specific needs and preferences. A personalized treatment plan that combines different interventions may be the most effective approach to manage knee osteoarthritis and help individuals regain mobility and improve their quality of life.
| Treatment Option | Description |
|---|---|
| Exercise Programs | Low-impact exercises to improve muscle strength and joint stability |
| Hyaluronic Acid Injections | Injections of a gel-like substance to provide lubrication and cushioning |
| Medication | Over-the-counter or prescription drugs to manage pain and inflammation |
| Physiotherapy | Customized exercise programs, manual therapy, and lifestyle modifications |
| Arthroscopic Surgery | Minimally invasive surgery to repair or remove damaged tissue |
| Arthroplasty (Joint Replacement Surgery) | Replacement of damaged knee joint parts with artificial components |
Potential Consequences of Knee Osteoarthritis
If knee osteoarthritis is left untreated or not properly managed, it can have various consequences that significantly impact an individual’s health and quality of life.
Excess weight can worsen symptoms and lead to obesity, which increases the risk of developing other health conditions such as diabetes and heart disease.
Obesity puts additional strain on the knee joints, exacerbating pain, inflammation, and joint degeneration. It also affects the overall well-being of individuals, impairing their ability to engage in physical activities and potentially leading to a sedentary lifestyle.
Individuals with knee osteoarthritis are also more prone to falls and fractures due to decreased joint function and muscle weakness.
As knee osteoarthritis progresses, the joint becomes less stable, making it easier for individuals to lose balance and experience falls. These falls can result in fractures, further compromising mobility and independence.
In severe cases, joint surgery, such as joint fusion or replacement, may be necessary to relieve pain and restore mobility.
Joint surgery is considered when conservative treatment options no longer provide relief or when there is significant joint damage. Surgical interventions aim to alleviate pain, improve joint function, and enhance the individual’s overall quality of life.
To prevent or minimize these potential consequences, it is essential to seek early diagnosis and adopt a comprehensive treatment plan that includes appropriate lifestyle changes, medications, physical therapy, and regular follow-up with healthcare professionals.
| Consequence | Description |
|---|---|
| Obesity | Excess weight worsens symptoms and increases the risk of developing other health conditions such as diabetes and heart disease. |
| Falls and Fractures | Decreased joint function and muscle weakness make individuals more prone to falls, which can result in fractures and further mobility issues. |
| Joint Surgery | In severe cases, joint surgery may be necessary to relieve pain and restore mobility when conservative treatment options are no longer effective. |
Conclusion
Knee osteoarthritis is a common degenerative joint disease that primarily affects the knee. Early recognition of the signs and symptoms is crucial for timely diagnosis and effective treatment. Ignoring knee osteoarthritis can have serious consequences, such as obesity and an increased risk of falls. Therefore, it is important to take the necessary steps to manage this condition and improve quality of life.
There are various treatment options available for knee osteoarthritis, including exercise programs, injections, medication, physiotherapy, and surgery. These treatments aim to alleviate symptoms, reduce pain, improve mobility, and prevent further joint damage. It is essential to seek medical attention and work with healthcare professionals to develop a personalized treatment plan that suits your specific needs and preferences.
By addressing knee osteoarthritis and following a comprehensive treatment plan, you can better manage the condition and minimize its impact on your daily life. It is also important to maintain a healthy lifestyle, including regular exercise, a balanced diet, and weight management, to reduce the risk of complications associated with knee osteoarthritis. Remember, early intervention and proactive management are key to effectively managing knee osteoarthritis and preserving joint function for the long term.
FAQ
What is knee osteoarthritis?
Knee osteoarthritis is a degenerative joint disease that primarily affects the knee. It is characterized by joint degeneration, leading to symptoms such as knee pain, stiffness, and swelling.
What are the symptoms of knee osteoarthritis?
The symptoms of knee osteoarthritis include knee pain, stiffness in the joint, clicking sounds, pain when touching a certain area of the knee, and joint deformities such as bony protrusions.
What causes knee osteoarthritis?
Knee osteoarthritis can be caused by joint wear and tear, age-related degeneration, previous knee injuries, an unhealthy diet leading to obesity, and underlying conditions such as rheumatoid arthritis or gout.
How is knee osteoarthritis diagnosed?
Knee osteoarthritis is typically diagnosed through a combination of medical history, physical examination, and imaging tests such as X-rays or MRIs. These tests help assess the extent of joint degeneration and rule out other potential causes of knee pain.
What are the treatment options for knee osteoarthritis?
Treatment options for knee osteoarthritis include exercise programs to improve muscle strength and joint stability, hyaluronic acid injections to relieve pain, medication to manage symptoms, physiotherapy to improve mobility, and surgery in severe cases.
What are the potential consequences of knee osteoarthritis?
Untreated knee osteoarthritis can lead to complications such as obesity, increased risk of falls, and the need for joint surgery to relieve pain and restore mobility.

Leave a Reply