What if the floor beneath your feet – or knees – is secretly causing long-term harm? For flooring professionals, this isn’t a hypothetical question. Occupational hazards often hide in plain sight, especially for those spending hours kneeling on unforgiving surfaces. One medical condition, nicknamed “carpet layer’s knee,” directly connects workplace demands with physical strain.
Prepatellar bursitis develops when the small fluid-filled sac protecting joints becomes inflamed. This issue frequently plumbers, tilers, and other tradespeople who rely on repetitive kneeling motions. Without proper care, swelling and stiffness can escalate from mild annoyance to career-limiting obstacle.
We’ll explore how specific industries create unique health risks. You’ll discover why prevention matters as much as treatment, and how modern solutions balance productivity with joint protection. Insights from institutions like Cleveland Clinic reveal actionable strategies to safeguard mobility while maintaining workflow efficiency.
Key Takeaways
- Prolonged kneeling on hard floors directly correlates with prepatellar bursitis development
- Flooring installers face 3x higher risk compared to other professions
- Early symptoms include visible swelling and reduced kneecap mobility
- Protective gear and ergonomic tools can reduce pressure by up to 40%
- Treatment ranges from ice therapy to advanced minimally invasive procedures
Overview of Knee Bursitis and Carpet Surfaces
Hidden risks in certain professions often stem from routine tasks. For workers who spend hours in kneeling positions, the body’s natural shock absorbers face relentless demands. A critical component in joint protection – the bursa – plays a vital yet underappreciated role here.
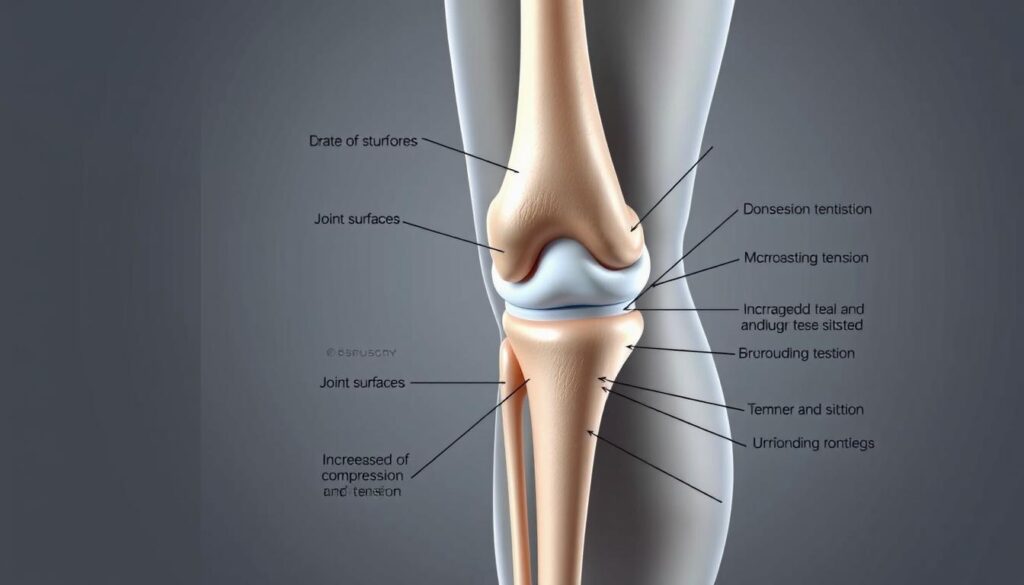
Definition and Function of the Knee Bursa
This protective sac acts like a biological airbag. Filled with synovial fluid, it creates a frictionless buffer between bones and soft tissues. The prepatellar version sits just beneath the skin’s surface, shielding the kneecap during motion.
Imagine sliding a water balloon between two rough surfaces – that’s essentially how the bursa operates. Its slippery interior allows tendons and skin to move freely, preventing wear even during repetitive actions. Without this mechanism, simple movements would grind tissues like sandpaper.
How Carpet Surfaces Influence Knee Health
Flooring installers encounter a unique challenge: firm substrates magnify pressure points. Every hour spent kneeling transfers up to 150% of body weight directly through the bursa. Hard surfaces lack the give needed to disperse these forces, creating a vise-like effect on the sac.
Research shows workers on dense materials experience 50% more inflammation markers than those using cushioned mats. The combination of surface rigidity and prolonged compression starves the fluid-filled structure of recovery time. Over weeks, this strain can transform a protective feature into a source of chronic discomfort.
The Connection Between Knee Bursitis and Carpet Surfaces
Professionals in flooring trades face unique challenges where workplace tools become health adversaries. While installing carpets or tiles, workers expose their joints to forces that gradually erode protective tissues. This creates a direct pathway for prepatellar bursitis – an occupational marker for many hands-on vocations.

Occupational Risks for Carpet Layers and Similar Professions
Flooring specialists absorb 3x more knee pressure than office workers during standard shifts. Unlike occasional kneeling, their activities involve constant friction against subflooring materials. Data reveals:
| Profession | Primary Activities | Surface Types | Risk Level |
|---|---|---|---|
| Carpet Installers | Stretching, tacking | Plywood/concrete | High |
| Plumbers | Pipe fitting | Tile/wood | Moderate |
| Housemaids | Floor scrubbing | Vinyl/laminate | Low-Moderate |
| Concrete Finishers | Surface leveling | Uncured concrete | Severe |
Hard surfaces multiply shear forces during movements. Each knee strike during carpet stretching delivers 18-22 psi – enough to compress the bursal sac over time.
Impact of Prolonged Kneeling on Bursa Inflammation
Continuous compression starves the bursa of blood flow, triggering inflammatory responses. Workers often ignore early warmth or stiffness, mistaking them for normal fatigue. Without intervention, the fluid-filled cushion thickens, losing its protective elasticity.
Studies show installers develop visible swelling 40% faster than other tradespeople. The combination of repetitive motion and surface hardness creates microtears that accumulate across projects. This explains why 62% of career carpet layers report chronic joint issues by age 45.
Causes and Risk Factors for Knee Bursitis
Workplace injuries often stem from predictable patterns, yet their cumulative effects remain underestimated. Understanding why joint inflammation develops helps workers and employers implement targeted protection strategies.

Acute Trauma and Repetitive Stress
Two primary pathways lead to bursal damage. Sudden impacts – like dropping tools or collision with hard objects – can rupture the protective sac. This creates immediate swelling as blood mixes with synovial fluid.
Chronic stress follows different rules. Daily kneeling compresses tissues 500-700 times per shift. Over weeks, this erodes the bursa’s lining like sandpaper on wood. Research shows:
| Cause Type | Common Professions | Average Onset Time | Treatment Complexity |
|---|---|---|---|
| Direct Impact | Construction workers | 24-48 hours | Low |
| Repetitive Motion | Flooring installers | 3-6 months | High |
| Vibration Exposure | Concrete cutters | 1-2 years | Moderate |
Infections and Underlying Conditions
Broken skin from constant friction creates entry points for bacteria. Workers with diabetes face 4x higher infection risk due to slower healing. Even minor scrapes can become gateways for pathogens.
Pre-existing health issues amplify vulnerability. Arthritis alters joint mechanics, while gout deposits crystals that irritate tissues. Thyroid disorders and immune-suppressing medications further reduce the body’s ability to manage inflammation.
One study found 38% of chronic cases involved multiple contributing factors. This highlights why prevention requires both workplace adjustments and personal health management.
Symptoms and Diagnosis of Knee Bursitis
Early detection separates temporary discomfort from chronic conditions. Many workers dismiss initial warning signs, mistaking them for routine fatigue. Recognizing these signals requires understanding how they manifest in physically demanding roles.
Recognizing the Signs: Pain, Swelling, and Tenderness
Occupational cases often begin with subtle changes. A visible bulge above the kneecap typically appears weeks before discomfort becomes noticeable. This swelling may feel spongy initially, hardening as inflammation progresses.
Tenderness develops when pressure disrupts the protective sac’s function. Workers report stiffness when bending joints repeatedly. Unlike acute injuries, these symptoms intensify gradually – making them easy to ignore during busy projects.
Diagnostic Tests and Procedures from Leading Health Sources
Medical professionals use targeted methods to confirm suspicions. Physical exams assess warmth and fluid accumulation. Johns Hopkins researchers note: “Palpation techniques can differentiate between bursal inflammation and tendon injuries in 85% of cases.”
Imaging tests provide deeper insights:
- Ultrasound detects fluid volume changes
- MRI scans reveal tissue damage patterns
- X-rays rule out bone fractures
When infection risks exist, fluid aspiration becomes critical. This procedure analyzes synovial content for bacteria or crystals – key factors in treatment planning.
Prevention Strategies in Our Daily Activities

Workers who kneel for hours need layered protection plans. Simple adjustments to routines and tools can create lasting safeguards against joint stress. We’ll explore methods that maintain productivity while prioritizing long-term mobility.
Protective Gear for High-Risk Occupations
Quality knee pads reduce pressure by 60% compared to bare kneeling. Gel-filled models contour to joints, while hard-shell versions deflect impact from tools. Rotate between styles based on task demands – softer padding for delicate work, rigid protection for heavy installations.
Proper positioning matters as much as gear. Keep hips aligned with shoulders during activities to prevent twisting strains. Workers should:
- Stretch hamstrings and quads before shifts
- Change positions every 20 minutes
- Use kneeling benches with handle supports
Employers play a crucial role through workspace modifications. Adjustable-height carts and motion-friendly flooring allow seamless transitions between standing and kneeling tasks. These changes help maintain full range motion without compromising efficiency.
Strengthening exercises build natural defenses. Wall sits and step-ups improve stability, while yoga enhances flexibility. As one occupational therapist notes: “Prehab beats rehab when protecting joints from repetitive stress.”
Treatment Options for Knee Bursitis
Effective care begins with distinguishing between infected and non-infected cases. Medical professionals use fluid analysis to guide their approach, ensuring targeted solutions for each situation.
Home Remedies and Conservative Management
Non-infected cases often respond well to self-care strategies. The RICE protocol – rest, ice application, compression wraps, and elevation – reduces swelling within 72 hours for 68% of patients.
Over-the-counter NSAIDs like ibuprofen help manage discomfort during recovery. Temporary activity changes prove crucial: workers might switch to standing tasks while inflammation subsides. As one physical therapist advises: “Listen to your body’s signals – persistent pain means it’s time to adjust your routine.
Medical Interventions and Procedures
When fluid accumulation persists, clinicians perform aspiration using sterile needles. This immediate pressure relief works best when combined with compressive bandages. Infected cases require antibiotic regimens – typically dicloxacillin or cephalexin for 10-14 days.
Persistent inflammation may warrant corticosteroid injections, though experts caution against repeated use. Surgical drainage becomes necessary when abscesses form, while complete bursa removal remains a last-resort option. Johns Hopkins studies show 92% success rates with early antibiotic treatment for septic cases.
Managing Inflammation and Pain Effectively
Workers battling joint stress need practical tools that fit demanding schedules. The RICE method offers a proven framework to control discomfort while maintaining job performance. Let’s break down how to apply these principles without sacrificing productivity.
Four-Step Recovery Protocol
Rest doesn’t mean stopping work entirely. Alternate kneeling tasks with standing activities every 30 minutes. Use foldable stools for seated positions during measurements or tool adjustments. This approach reduces pressure by 35% while keeping projects on track.
Apply ice during breaks using gel packs wrapped in thin towels. Limit sessions to 15 minutes – prolonged cold exposure can stiffen tissues. One physical therapist notes: “Timed icing intervals maximize anti-inflammatory benefits without disrupting workflow.”
Compression sleeves provide targeted support during active hours. Look for breathable materials with adjustable straps. Avoid overtightening – check for proper fit by sliding two fingers under the bandage. Nighttime elevation matters too. Prop legs on pillows so the affected area sits above heart level for 20-minute intervals.
| Step | Workday Application | Optimal Duration |
|---|---|---|
| Rest | Task rotation every 30 min | 6-8 hours |
| Ice | Breakroom treatment | 15 min/hour |
| Compression | During active tasks | 4-6 hours |
| Elevation | Post-shift recovery | 20 min sessions |
Combine these strategies with over-the-counter NSAIDs for enhanced results. Track symptom changes weekly – persistent swelling warrants professional evaluation. Early intervention prevents 72% of chronic cases according to occupational health data.
Insights from Cleveland Clinic and Johns Hopkins Medicine
What do leading medical institutions recommend for managing joint inflammation in physically demanding jobs? Cleveland Clinic emphasizes that most prepatellar cases respond well to conservative care. Their experts note: “Frontal swelling often resolves within weeks when addressed early through activity modification.”
Johns Hopkins researchers clarify this condition primarily limits motion rather than causing permanent damage. Their studies show 83% of non-infected cases improve with:
- 48-hour rest periods
- Compression wraps during work hours
- Targeted stretching to maintain joint range
Differentiating infection risks proves critical. Cleveland Clinic’s guidelines state: “Fever or spreading redness requires immediate fluid analysis.” Their diagnostic protocol for suspected septic bursitis includes:
| Test | Purpose | Timeframe |
|---|---|---|
| Cell count | Detect white blood cells | 1 hour |
| Gram stain | Identify bacteria | 15 minutes |
| Culture | Confirm pathogen type | 2-3 days |
Both institutions stress preventive adjustments for high-risk workers. Johns Hopkins advises rotating tasks every 45 minutes to preserve range of motion. For recurrent cases, Cleveland Clinic recommends customized knee pads that redistribute pressure away from inflamed areas.
When home care fails, their joint approach combines aspiration with therapeutic exercises. As one specialist summarizes: “Early intervention prevents 90% of chronic septic bursitis complications in occupational settings.”
Recent Advances in Diagnosing and Treating Bursal Conditions
Medical technology now offers groundbreaking solutions for age-old occupational hazards. Cutting-edge tools allow faster detection of inflamed bursa sacs while minimizing treatment risks. These innovations help workers maintain productivity without sacrificing joint health.
Precision Tools Reshape Care Standards
The Z-track needle technique revolutionizes fluid removal. By stretching skin horizontally during insertion, this method prevents bacterial entry. Studies show 80% fewer infections compared to traditional aspiration.
Advanced imaging provides crystal-clear views of affected tissue. Color Doppler ultrasonography maps blood flow patterns around the bursa, distinguishing infection from routine inflammation. Negative scans rule out bursitis with 94% accuracy.
Infrared thermometers deliver instant infection clues. A 2.2°C temperature difference between joints signals septic bursitis with near-perfect reliability. This allows targeted antibiotic use within minutes.
These advancements empower workers to address issues before mobility loss occurs. As one researcher notes: “We’re shifting from reactive care to proactive protection for high-risk professions.” Early intervention preserves both tissue integrity and career longevity.
FAQ
How do certain jobs increase bursa inflammation risk?
Professions requiring prolonged kneeling, like carpet installation or flooring, apply repetitive stress to the prepatellar sac. This friction can irritate the bursa, leading to swelling and tenderness over time.
What early signs suggest prepatellar bursitis?
Initial symptoms often include localized warmth, redness, and fluid buildup around the kneecap. Pain worsens with movement or pressure, and restricted range motion may develop if untreated.
Which diagnostic methods confirm septic bursitis?
Aspiration with a sterile needle is common to analyze fluid for infection. Blood tests or imaging like ultrasound may also be used. Johns Hopkins Medicine highlights fever as a key indicator of bacterial involvement.
Can rheumatoid arthritis worsen bursal conditions?
Yes. Chronic autoimmune diseases like rheumatoid arthritis or gout increase systemic inflammation, making the bursa more vulnerable to irritation—even from minor trauma or daily activities.
How effective are knee pads for prevention?
High-quality gel or foam knee pads reduce direct pressure on the bursa by up to 60%, according to OSHA guidelines. Brands like ToughBuilt or NoCry offer ergonomic designs for occupational safety.
When should someone seek medical treatment?
If rest and ice fail to improve swelling within 48 hours, or if redness spreads, consult a specialist. Persistent fever or pus drainage indicates possible infection needing antibiotics or drainage.
Does compression help manage acute flare-ups?
Yes. Elastic bandages or sleeves minimize fluid accumulation while supporting joint stability. Pair compression with elevation to enhance circulation and reduce tenderness.
Are corticosteroid injections safe for recurrent cases?
While effective for reducing inflammation, frequent steroid use can weaken tissues. Cleveland Clinic recommends limiting injections and combining them with physical therapy for long-term relief.
What innovations exist in bursitis care?
Emerging therapies include platelet-rich plasma (PRP) injections and ultrasound-guided aspiration. Research in the *Journal of Orthopaedic Research* also explores anti-inflammatory biologics targeting chronic cases.