Have you ever experienced a dull ache in your knee that seems to coincide with your menstrual cycle? You’re not alone. Many women report heightened discomfort during certain phases of their cycle, leaving them wondering if there’s a connection between their hormonal fluctuations and joint pain.
Research suggests that female hormone levels are related to increased knee joint laxity and decreased stiffness at ovulation. As we explore this phenomenon, we’ll examine how changes in our cycle can impact joint stability and potentially lead to discomfort, shedding light on what this means for our overall health.
We’ll delve into the scientific evidence behind this connection and provide practical insights for women experiencing cycle-related knee pain.
Key Takeaways
- Understanding the link between the menstrual cycle and knee pain
- The role of hormonal fluctuations in joint stability
- Why many women experience knee pain during ovulation
- Practical insights for managing cycle-related knee pain
- When to seek medical attention for knee pain
The Connection Between Hormones and Joint Pain
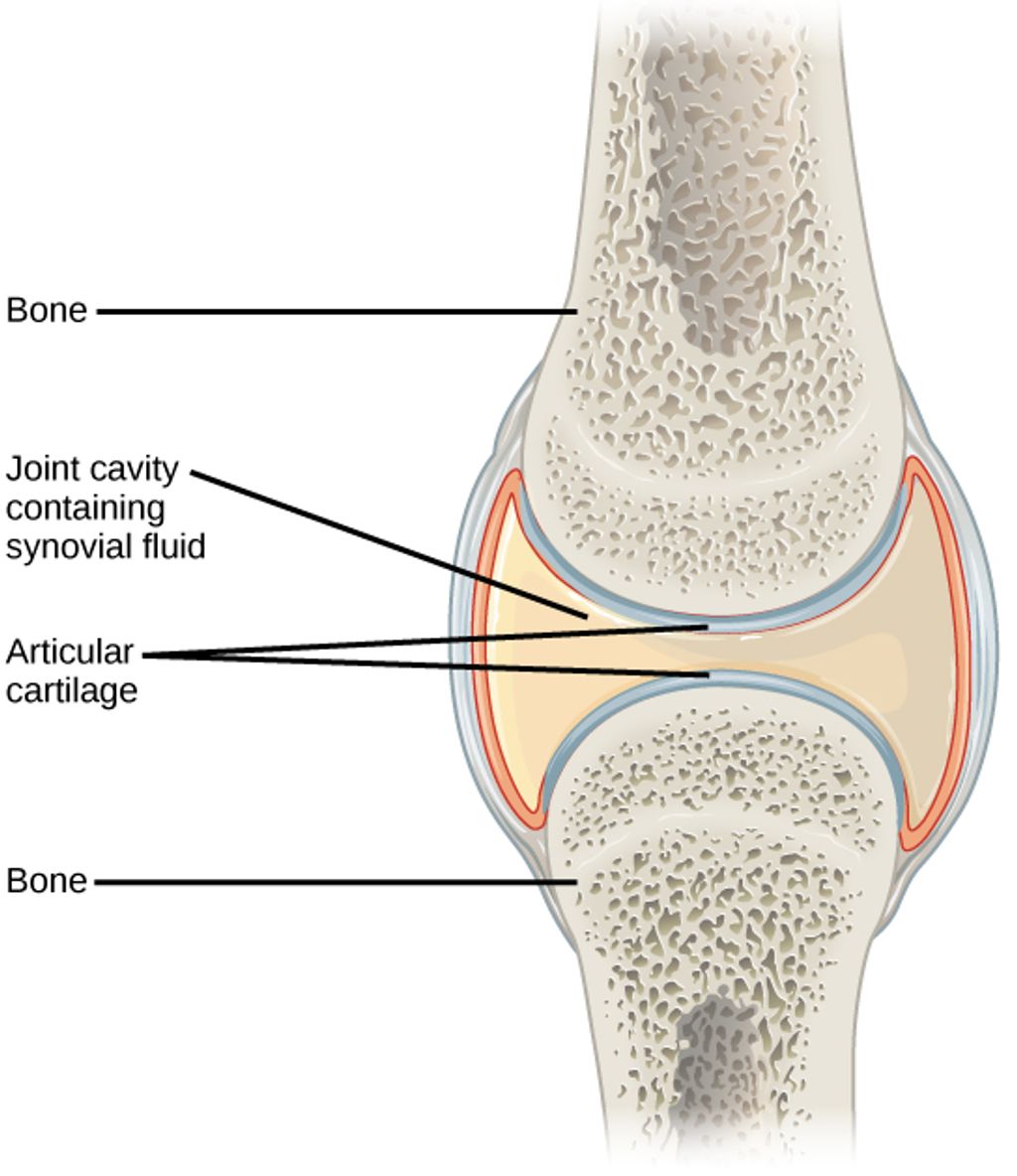
Understanding the link between reproductive hormones and joint health can provide insights into managing knee pain during ovulation. The menstrual cycle, which is regulated by hormones such as estrogen and progesterone, has a significant impact on various bodily functions beyond reproduction.
How Estrogen and Progesterone Affect Our Joints
Estrogen and progesterone are known to play crucial roles in fertility, but they also directly impact joint health. Estrogen’s anti-inflammatory properties can protect our joints when its levels are high. However, fluctuations in estrogen levels throughout the menstrual cycle can lead to varying degrees of joint comfort. Progesterone affects collagen synthesis and joint stability, particularly during different phases of the menstrual cycle.
The Menstrual Cycle’s Impact on Our Body
During the menstrual cycle, particularly in the luteal phase, levels of estrogen and progesterone fluctuate significantly. These hormonal changes influence not just the reproductive system but create systemic changes throughout our body, including our musculoskeletal system. As a result, women may experience changes in joint pain perception and inflammation levels.
The correlation between hormonal changes and joint symptoms can help us understand the timing of knee pain during ovulation. By examining the typical hormonal pattern throughout a 28-day cycle, we can better comprehend how these fluctuations affect joint health.
Understanding Knee Pain During Ovulation
As women navigate their menstrual cycle, some may experience knee pain during ovulation due to hormonal fluctuations. This discomfort can be attributed to the changes in hormone levels, particularly the surge in estrogen, which affects joint stability.
Why Ovulation Phase Can Trigger Joint Discomfort
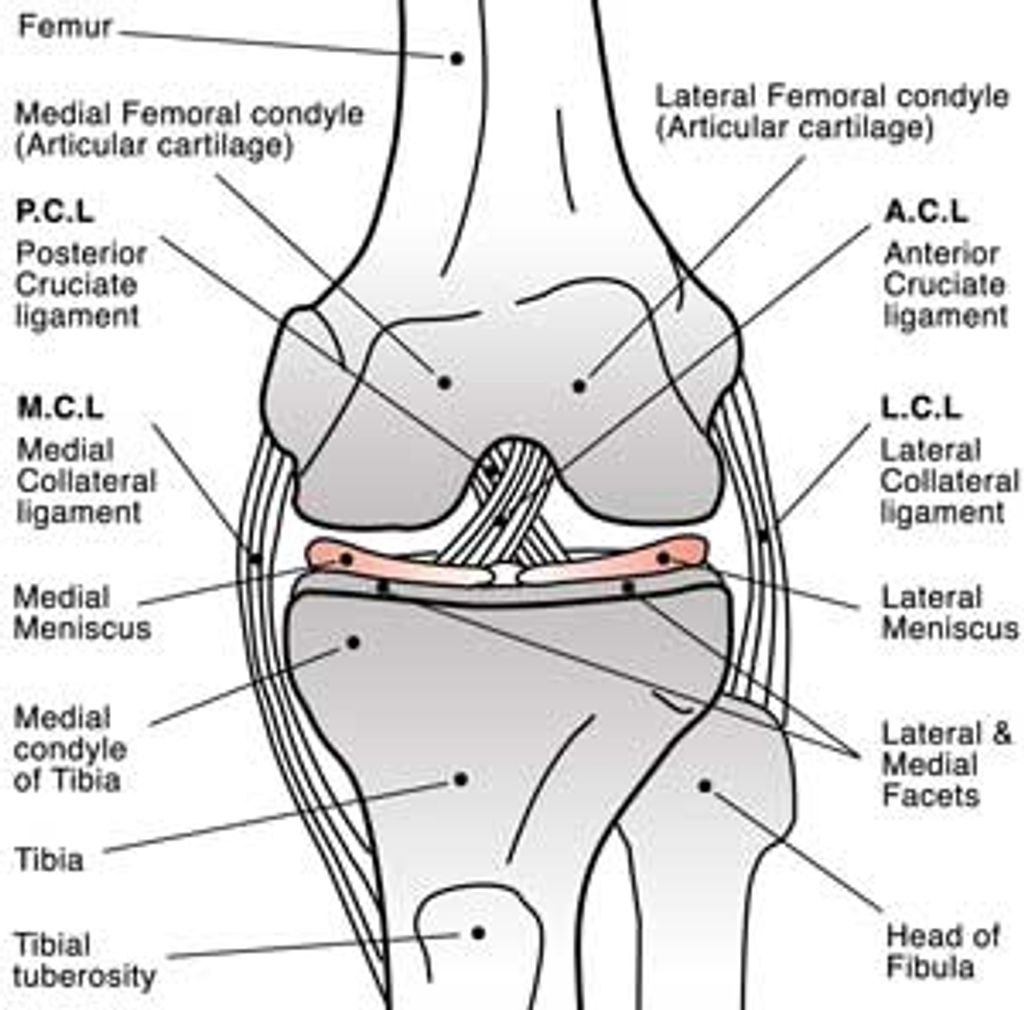
During the ovulation phase, the body undergoes significant hormonal changes. The increase in estrogen levels can lead to increased laxity in the knee joint. This is because estrogen affects the ligaments surrounding the knee, making them more susceptible to injury and discomfort.
- The surge in estrogen during ovulation impacts knee joint stability.
- Research has shown that knee laxity is more pronounced during ovulation compared to other phases of the menstrual cycle.
The Science Behind Increased Knee Laxity
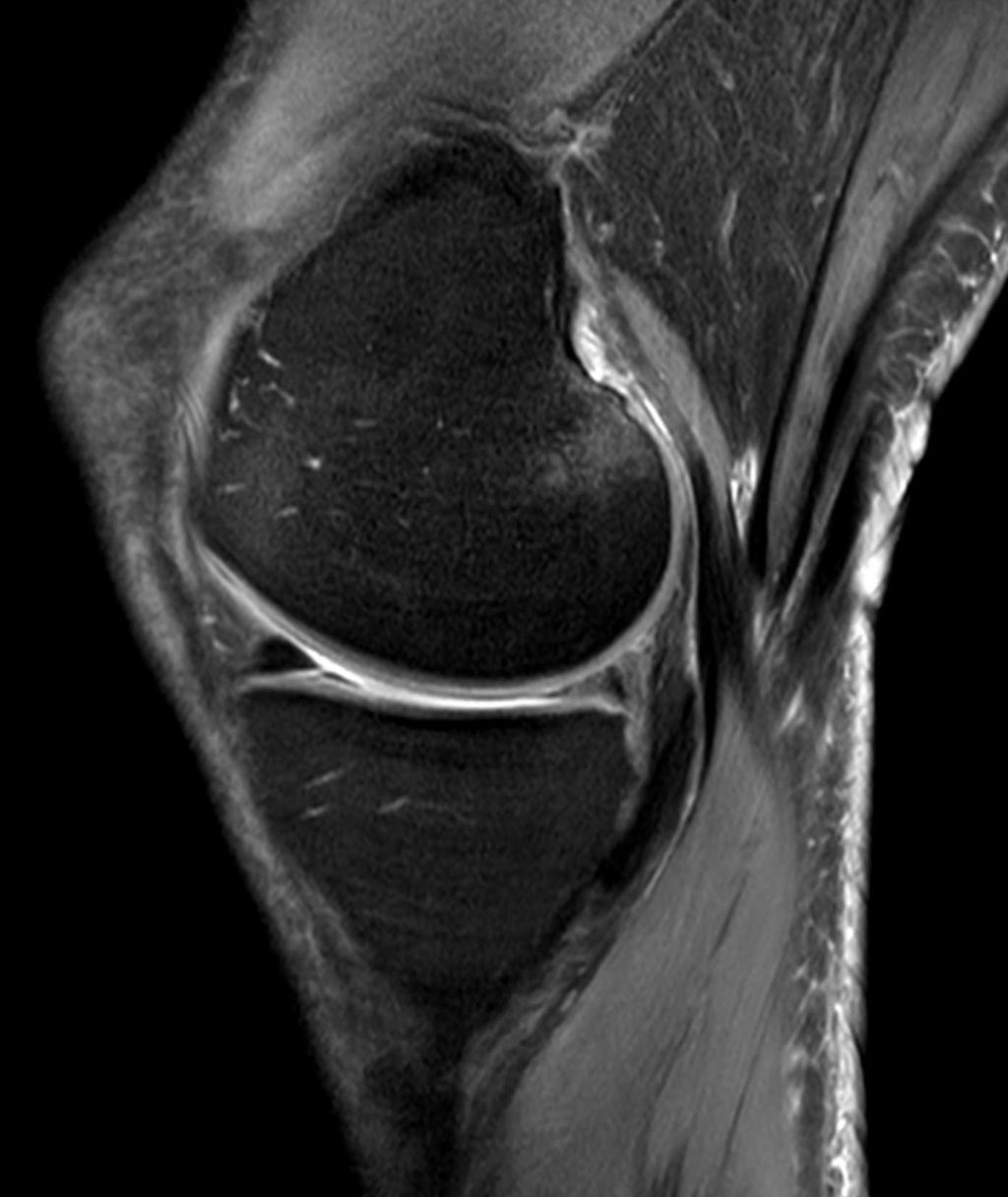
Studies have demonstrated that knee laxity is indeed greater during ovulation. For instance, one study found greater laxity at 89 N during ovulation (5.13 +/- 1.70 mm) compared to the luteal phase (4.55 +/- 1.54 mm), with a P-value of .012. Moreover, a reduction in knee stiffness of approximately 17% was observed during ovulation.
This increased laxity and reduced stiffness can create sensations of instability and pain for many women. Understanding these changes can help in managing knee pain during ovulation.
Research Findings on Hormonal Effects on Knee Stability
A comprehensive review of existing literature reveals the impact of hormonal changes on knee stability. Research in this area has focused on understanding how different phases of the menstrual cycle affect knee laxity.
Studies on Knee Laxity Throughout the Menstrual Cycle
Numerous studies have investigated knee laxity throughout the menstrual cycle. After a thorough literature search and review, 19 studies were included, comprising a total of 573 subjects. Eleven of these studies focused on athletes. The studies utilized a KT2000 or KT1000 arthrometer to measure knee laxity.
The female menstrual cycle was divided into follicular, ovulatory, and luteal phases for analysis. The findings indicated that the largest mean effect was observed between the ovulatory and follicular phases. Specifically, laxity of the anterior knee was greater during the ovulatory phase compared to the follicular phase by 0.40 ± 0.29 mm.
| Phase Comparison | Mean Difference in Knee Laxity (mm) |
|---|---|
| Ovulatory vs. Follicular | 0.40 ± 0.29 |
| Luteal vs. Follicular | 0.21 ± 0.21 |
Differences in Knee Stiffness During Various Cycle Phases
The research also highlighted differences in knee stiffness during various cycle phases. Anterior knee laxity was found to be greater in the luteal phase compared to the follicular phase by 0.21 ± 0.21 mm. These findings suggest that knee laxity varies significantly across different phases of the menstrual cycle.
Systematic reviews and meta-analyses have consolidated findings across multiple studies, providing more reliable conclusions about the relationship between cycle phases and knee laxity. By understanding these changes, researchers and healthcare professionals can better address knee-related issues in women.
Why Women Experience More Knee Injuries Than Men
Epidemiological data indicates a notable sex disparity in knee injury rates among athletes. Specifically, female athletes face a 2-4 times higher risk of ACL injuries compared to their male counterparts. This disparity is not observed in all types of knee injuries, suggesting specific mechanisms are at play.
The 2-4 Times Higher Risk of ACL Injuries in Female Athletes
Research has shown that female athletes are more likely to suffer ACL, particularly in sports that involve pivoting, jumping, and sudden directional changes. The reasons for this increased risk are multifactorial, involving a combination of anatomical, biomechanical, and hormonal factors.
Anatomical and Hormonal Contributing Factors
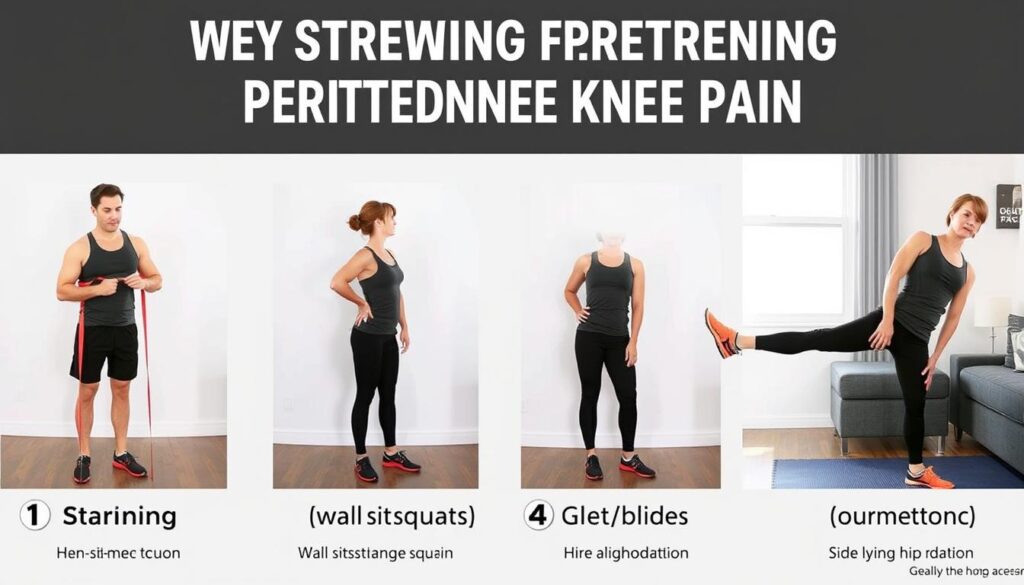
Anatomical differences, such as wider pelvises and smaller intercondylar notches in women, contribute to the increased risk. Additionally, hormonal fluctuations throughout the menstrual cycle may affect knee laxity and stability, further increasing the risk of injury. Understanding these factors has led to the development of specialized training protocols aimed at reducing injury risk in female athletes through targeted strengthening and neuromuscular training.
By examining the factors that contribute to the sex disparity in knee injuries, we can better understand why female athletes are more prone to certain types of injuries and develop effective prevention strategies.
The Paradox: Increased Laxity vs. Injury Risk
A closer examination of the menstrual cycle reveals an intriguing discrepancy between knee laxity and the risk of ACL injuries. Despite increased knee laxity during ovulation, research suggests that the risk of ACL injuries is not directly correlated with laxity levels across different cycle phases.
The menstrual cycle’s influence on knee stability is complex, involving fluctuations in hormone levels that affect ligament laxity and strength. Understanding this paradox is crucial for developing effective prevention and treatment strategies for ACL injuries.
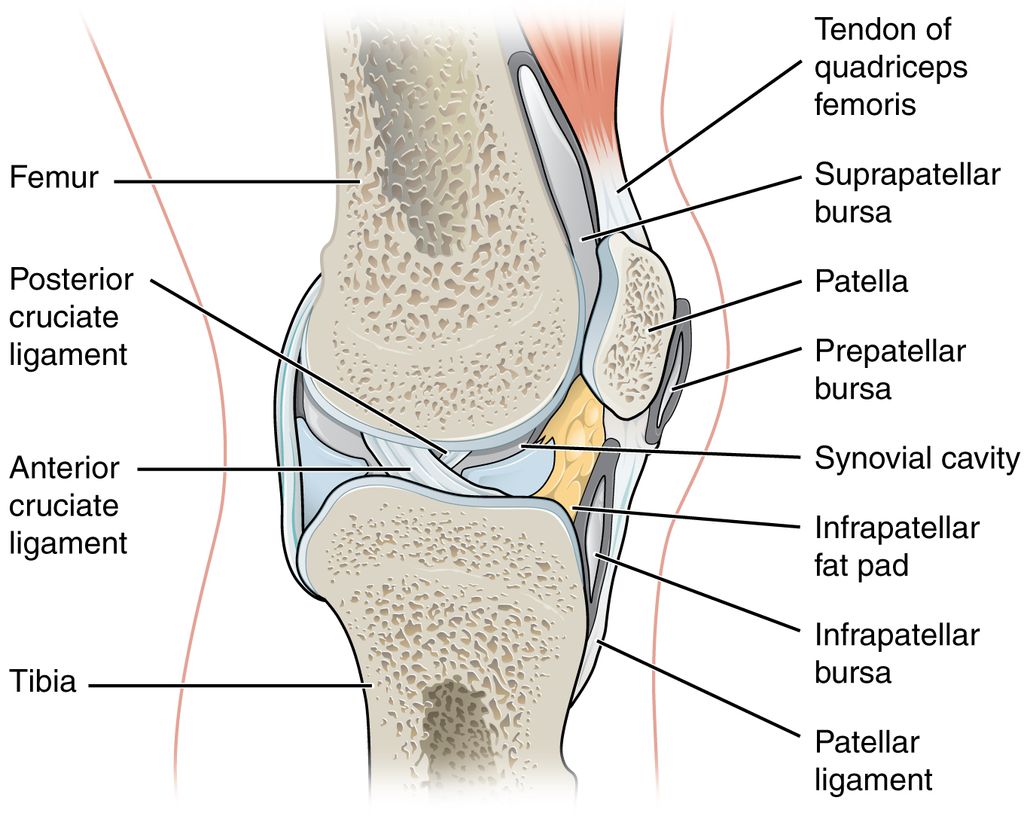
Why Follicular Phase May Present Higher Injury Risk
The follicular phase, characterized by rising estrogen levels, may present a higher risk for ACL injuries. This is potentially due to the effects of estrogen on ligament integrity. Increased estradiol during this phase can lead to decreased fibroblast activity and collagen synthesis, resulting in stiffer but structurally weaker ligaments.
- The follicular phase is marked by a significant increase in estrogen levels.
- This hormonal shift can affect ligament laxity and strength.
- The resulting ligaments may be stiffer but more prone to injury due to reduced collagen synthesis.
The Protective Role of Progesterone in the Luteal Phase
In contrast, the luteal phase, marked by a rise in progesterone, may offer protective effects against ACL injuries. Progesterone is believed to increase fibroblast activity and enhance collagen synthesis, potentially strengthening the ACL ligament. This hormonal shift could explain the lower incidence of ACL injuries during the luteal phase despite the presence of increased laxity.
- The luteal phase is characterized by increased progesterone levels.
- Progesterone promotes fibroblast activity and collagen synthesis.
- This can lead to stronger ligaments and a reduced risk of ACL tears.
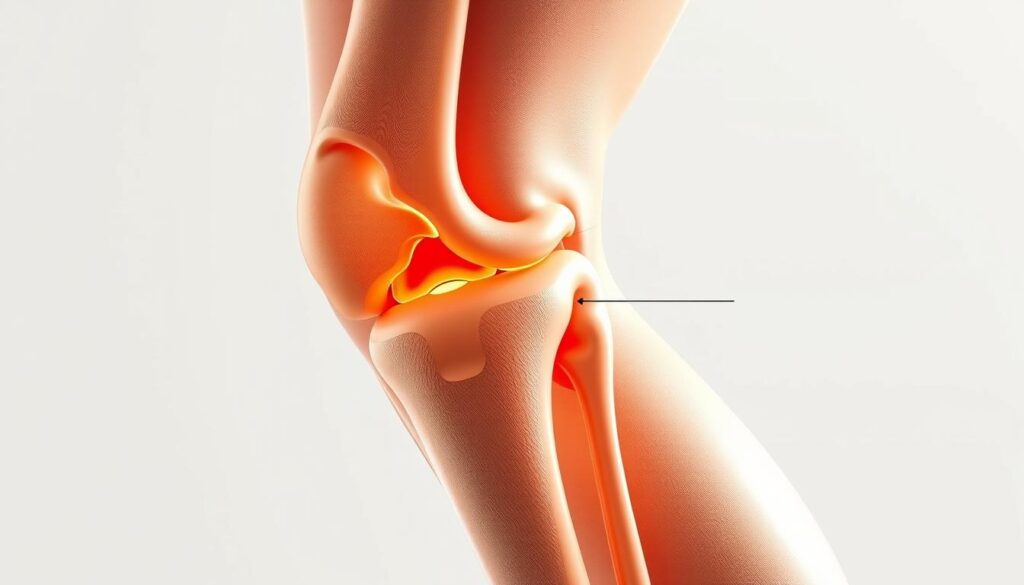
Recognizing Symptoms of Hormone-Related Knee Pain
The connection between hormonal fluctuations and knee pain is becoming increasingly recognized, with many women reporting cycle-related joint discomfort. This phenomenon is not just about pain; it encompasses a range of symptoms that can significantly impact daily life and athletic performance.
Common Experiences Reported by Women
Women often describe experiencing knee pain that predictably occurs around the same time each month, often intensifying during ovulation or in the days before menstruation begins. The pain can manifest as sensations of instability, aching, or changes in mobility. Many report that the intensity of the pain can vary, with some describing it as a 9 out of 10 on the pain scale during particularly difficult days.
Distinguishing Hormonal Pain from Other Knee Issues
Distinguishing hormone-related knee pain from other knee conditions requires careful consideration of timing patterns, accompanying symptoms, and response to treatments. Women experiencing knee pain related to their menstrual cycle may also report other symptoms such as lower back pain or joint discomfort throughout their body. Understanding these patterns can help in identifying whether the knee pain is hormone-related or due to another cause.
Managing Knee Pain During Ovulation
Understanding and managing knee pain during ovulation involves recognizing the intricate relationship between hormonal fluctuations and joint health. As we navigate our menstrual cycle, various physiological changes occur that can impact our joints, particularly the knee.
Tracking Symptoms Throughout Your Cycle
Keeping a detailed journal of your joint pain, including when it flares up, can help identify patterns. This information can be invaluable when discussing your symptoms with a healthcare provider. We can use cycle tracking apps or simple calendar methods to monitor our symptoms throughout our cycle, allowing us to predict when knee pain might worsen.
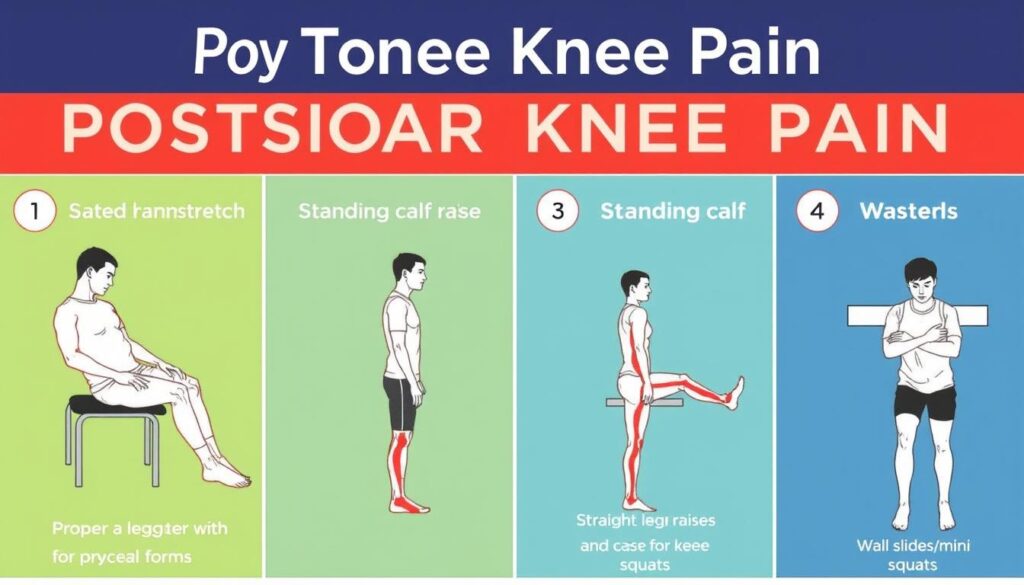
Physical Therapy and Exercise Approaches
Engaging in physical therapy can help strengthen muscles around the joints, improving stability and reducing pain. A physical therapist can design a personalized program tailored to our needs. Incorporating regular low-impact exercise, such as swimming or walking, can help maintain joint health. Strengthening the muscles surrounding the knee joint provides additional support during vulnerable phases of our cycle.
| Exercise | Benefits |
|---|---|
| Swimming | Low-impact, improves joint mobility |
| Walking | Strengthens surrounding muscles, improves stability |
| Physical Therapy | Personalized exercises to strengthen knee muscles |
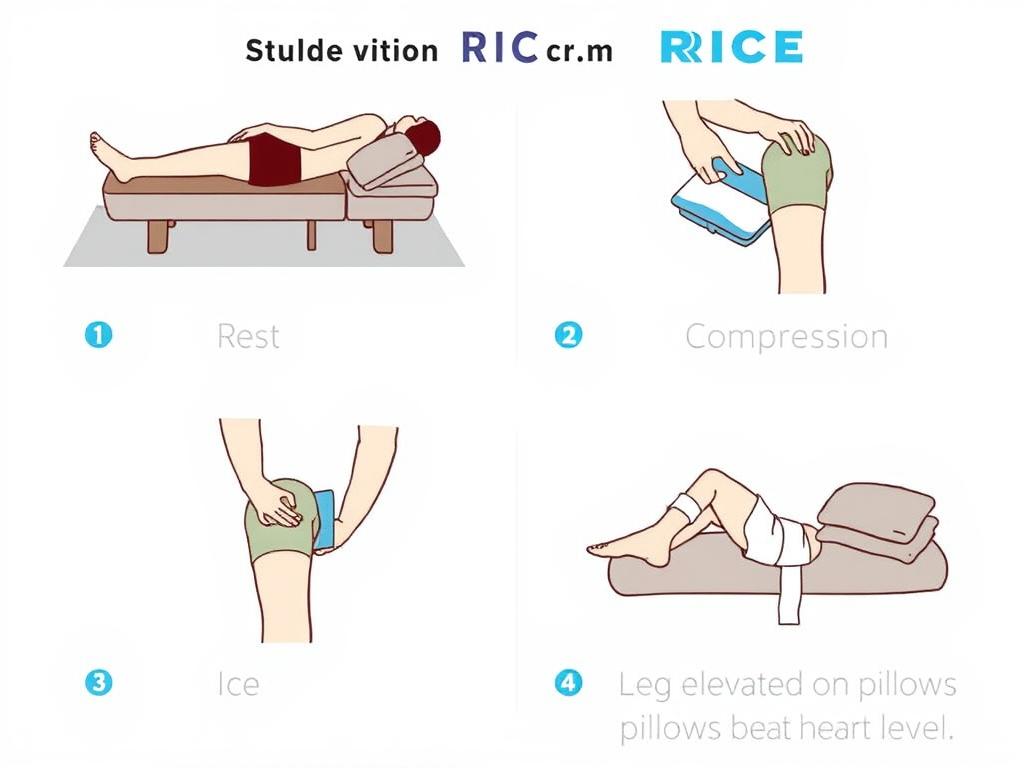
Medical Interventions and Pain Relief Options
For some women, medical interventions such as nonsteroidal anti-inflammatory drugs (NSAIDs) can provide relief for joint pain. Hormonal birth control methods may help stabilize fluctuations that contribute to joint pain. A balanced diet rich in omega-3 fatty acids and antioxidants may also help reduce inflammation.
By combining these approaches—tracking symptoms, engaging in physical therapy and appropriate exercises, and exploring medical interventions—we can effectively manage knee pain during ovulation and improve our overall quality of life.
When to Seek Professional Help for Cycle-Related Knee Pain
Recognizing the signs that suggest cycle-related knee pain requires medical attention can significantly impact treatment outcomes. If your knee pain is severe and interferes with your daily activities, it’s crucial to consult with a healthcare provider.
Warning signs that indicate the need for professional evaluation include pain that significantly impacts daily activities or doesn’t follow the expected pattern related to your menstrual cycle. To facilitate accurate diagnosis, it’s helpful to track and share information about your symptoms with your healthcare provider.
Healthcare providers may use various diagnostic methods, including hormone level testing, imaging studies, and physical examinations, to determine the cause of knee pain. Researchers emphasize the need for more high-quality studies to understand the effects of hormone changes on joint health better.
Fertility awareness-based methods (FABMs) can be valuable tools for tracking cycle phases in relation to knee symptoms, offering more precise data than calendar-based methods. By understanding the relationship between your menstrual cycle and knee pain, you can work with your healthcare provider to develop an effective treatment plan.
Women can play a crucial role in advancing research by participating in studies that investigate the relationship between hormone levels and joint health. By seeking professional help when needed and contributing to research, women can take proactive steps towards managing cycle-related knee pain and improving overall health.
FAQ
How do hormonal changes during the menstrual cycle affect our joints?
We know that fluctuations in estrogen and progesterone levels can impact our joints, particularly in the luteal phase and follicular phase. Research suggests that these hormonal changes can lead to increased knee laxity and stiffness.
Why do female athletes experience a higher risk of ACL injuries?
Studies have shown that female athletes are 2-4 times more likely to suffer from ACL injuries due to a combination of anatomical and hormonal factors. The changes in estrogen and progesterone levels throughout the menstrual cycle can contribute to this increased risk.
Can tracking symptoms throughout the menstrual cycle help manage knee pain?
Yes, we recommend tracking symptoms to identify patterns and correlations between hormonal changes and knee discomfort. This can help us develop a more effective plan to manage knee pain.
What are some common experiences reported by women with hormone-related knee pain?
Women often report increased knee stiffness and discomfort during certain phases of their menstrual cycle. We also note that some women experience more severe symptoms, such as joint laxity, which can increase the risk of injury.
Are there any effective ways to manage knee pain during ovulation?
We suggest exploring various approaches, including physical therapy, exercise, and medical interventions. By understanding the underlying causes of knee pain and working with healthcare professionals, we can develop a personalized plan to alleviate symptoms.
When should I seek professional help for cycle-related knee pain?
If we experience persistent or severe knee pain, it’s essential to consult with a healthcare professional to rule out underlying conditions and develop an effective treatment plan. They can help us determine the best course of action to manage symptoms and prevent future injuries.