Knee Cartilage Degeneration: Causes, Symptoms, and Treatment Options
Knee cartilage degeneration is a common condition that affects millions of people worldwide. It occurs when the cartilage that cushions the knee joint begins to wear away, leading to pain, stiffness, and limited mobility. While this condition can occur at any age, it is more common in older adults and athletes who put a lot of stress on their knees.

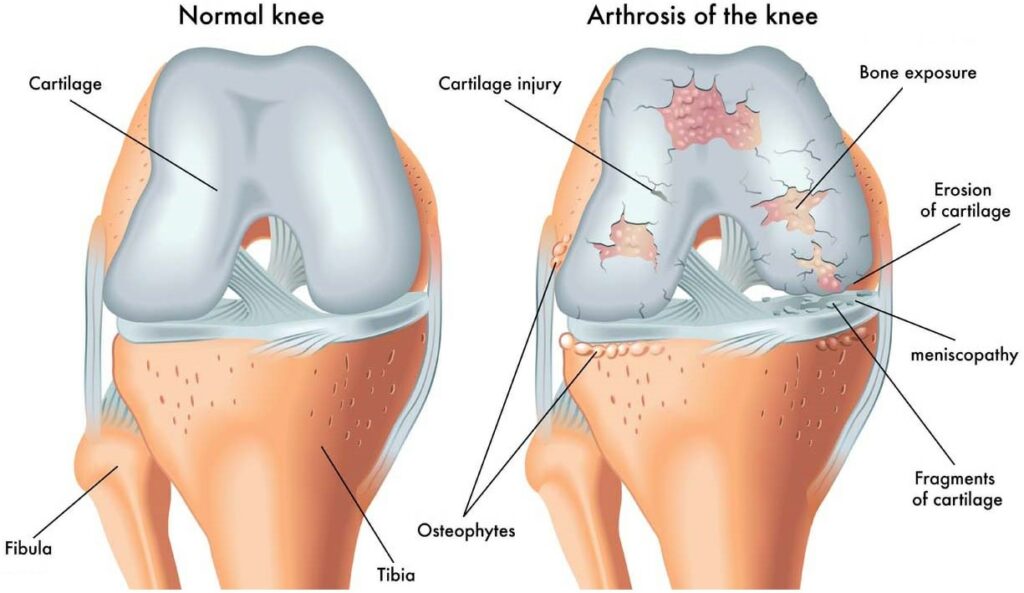
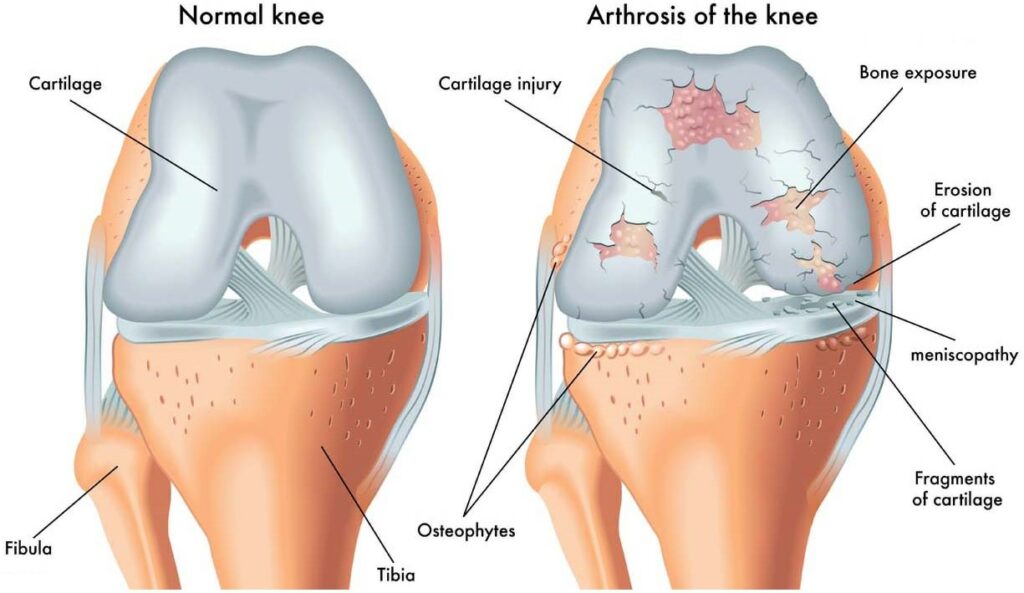
Understanding Knee Cartilage Degeneration is important for anyone who wants to maintain healthy knees. The knee joint is made up of three bones: the femur, tibia, and patella. Between these bones is a layer of cartilage that acts as a shock absorber, preventing the bones from rubbing against each other. When this cartilage begins to break down, it can cause pain and inflammation in the knee joint. There are several factors that can contribute to knee cartilage degeneration, including age, genetics, obesity, and injury.
If left untreated, knee cartilage degeneration can lead to more serious complications, such as osteoarthritis. Fortunately, there are several treatment options available to manage this condition, including physical therapy, medication, and surgery. By taking proactive steps to prevent knee cartilage degeneration and seeking prompt treatment when symptoms arise, individuals can maintain healthy knees and enjoy an active lifestyle for years to come.
Key Takeaways
- Knee cartilage degeneration is a common condition that affects the knee joint and can cause pain, stiffness, and limited mobility.
- Factors that contribute to knee cartilage degeneration include age, genetics, obesity, and injury.
- Treatment options for knee cartilage degeneration include physical therapy, medication, and surgery, and early intervention can help prevent more serious complications.
Understanding Knee Cartilage Degeneration
Knee cartilage degeneration is a common condition that occurs when the cartilage in the knee joint wears away. This can lead to pain, swelling, and stiffness in the knee, making it difficult to perform daily activities.
Causes of Degeneration
There are several factors that can contribute to knee cartilage degeneration. Osteoarthritis is a common cause, which occurs when the articular cartilage that covers the ends of the tibia and femur bones in the knee joint breaks down over time. This can be due to aging, injury, trauma, wear and tear, or genetics.
Other factors that can contribute to knee cartilage degeneration include joint damage, physical activity, and obesity. In some cases, there may be no obvious cause for the degeneration.
Symptoms and Diagnosis
The symptoms of knee cartilage degeneration can vary depending on the severity of the condition. Common symptoms include knee pain, swelling, stiffness, and limited range of motion. In some cases, there may be a clicking or popping sound when the knee is moved.
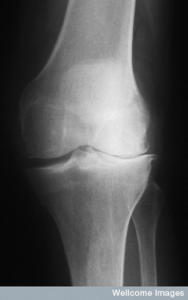
Diagnosis of knee cartilage degeneration typically involves a physical exam, medical history, and diagnostic tests such as x-rays and magnetic resonance imaging (MRI). These tests can help to identify the extent of the damage and determine the best course of treatment.
Overall, understanding the causes and symptoms of knee cartilage degeneration is important for managing the condition and preventing further damage to the knee joint. If you are experiencing knee pain or other symptoms, it is important to seek medical attention and discuss your treatment options with your healthcare provider.
Risk Factors and Complications

Knee cartilage degeneration can be caused by several risk factors that increase the likelihood of developing the condition. In this section, we will discuss identifying risk factors and potential complications associated with knee cartilage degeneration.
Identifying Risk Factors
The following factors may increase the risk of knee cartilage degeneration:
- Age: Cartilage naturally wears down over time, making older adults more susceptible to the condition.
- Gender: Women are more likely than men to develop knee cartilage degeneration.
- Obesity: Excess weight puts additional pressure on the knees, which can lead to cartilage damage.
- Previous injury: A history of knee injuries can increase the risk of developing knee cartilage degeneration.
- Occupation: Jobs that require repetitive knee movements, such as construction work, can increase the risk of developing the condition.
Potential Complications
Knee cartilage degeneration can lead to several complications, including:
- Joint damage: As cartilage wears down, bones in the knee may rub against each other, causing joint damage.
- Disability: Severe cases of knee cartilage degeneration can limit mobility and lead to disability.
- Instability: As cartilage wears down, the knee joint may become unstable, making it more difficult to walk or stand.
- Medical conditions: Knee cartilage degeneration can increase the risk of developing other medical conditions, such as diabetes and fever.
- Deformities: In some cases, knee cartilage degeneration can cause the knee joint to become misaligned or deformed.
Overall, understanding the risk factors and potential complications associated with knee cartilage degeneration is important for early detection and treatment of the condition.
Treatment and Management
When it comes to knee cartilage degeneration, there are a variety of treatment options available. The best course of action will depend on the severity of the condition, as well as the individual needs and goals of the patient.
Non-Surgical Treatments
For those with mild to moderate knee cartilage degeneration, non-surgical treatments may be effective. These can include:
- Physical therapy: This can help improve mobility and flexibility, as well as strengthen the muscles around the knee joint.
- Medications: Anti-inflammatory drugs such as NSAIDs or corticosteroids can help reduce inflammation and pain.
- Injections: Platelet-rich plasma (PRP) or hyaluronic acid injections may be used to promote healing and reduce pain.
- Braces: Knee braces can help stabilize the joint and reduce pain during physical activity.
Surgical Treatments
In more severe cases of knee cartilage degeneration, surgical treatments may be necessary. These can include:
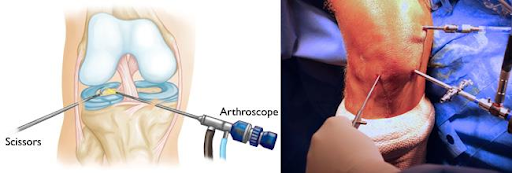
- Arthroscopy: This minimally invasive procedure involves inserting a small camera into the knee joint to remove damaged tissue or bone spurs.
- Autologous chondrocyte implantation: This procedure involves removing healthy cartilage cells from the patient’s knee, growing them in a lab, and then implanting them back into the knee joint to promote healing.
- Joint replacement surgery: This involves removing the damaged knee joint and replacing it with an artificial joint.
It’s important to note that surgery is generally considered a last resort, and conservative treatment options should be exhausted before considering surgical intervention.
If you are experiencing knee pain, redness, or swelling, or if you are having difficulty with mobility or flexibility in your knee joint, it’s important to see a doctor. They can help diagnose the underlying cause of your symptoms and recommend appropriate treatment options.
Prevention is also key when it comes to knee cartilage degeneration. Maintaining a healthy weight, avoiding repetitive stress on the knee joint, and engaging in regular exercise can all help prevent degenerative joint disease from developing.
Frequently Asked Questions

What are the early symptoms of knee arthritis?
The early symptoms of knee arthritis include pain, stiffness, and swelling in the knee joint. You may also experience a decrease in range of motion and difficulty walking. If you are experiencing any of these symptoms, it is recommended that you see a doctor for an evaluation.
What are some new treatments for osteoarthritis of the knee?
There are several new treatments for osteoarthritis of the knee, including stem cell therapy, platelet-rich plasma (PRP) therapy, and hyaluronic acid injections. These treatments can help to reduce pain, inflammation, and promote healing of damaged cartilage.
What causes degeneration of cartilage?
Degeneration of cartilage can be caused by a variety of factors, including aging, injury, and genetics. Other factors that can contribute to cartilage degeneration include obesity, repetitive stress on the joints, and certain medical conditions such as rheumatoid arthritis.
Can knee arthritis pain radiate down the leg?
Yes, knee arthritis pain can radiate down the leg. This is because the nerves that supply sensation to the knee joint also supply sensation to other parts of the leg, such as the thigh and calf.
What are the symptoms of having no cartilage in the knee?
The symptoms of having no cartilage in the knee include pain, swelling, stiffness, and a decrease in range of motion. You may also experience a grinding or popping sensation when you move your knee.
How can knee cartilage damage be treated effectively?
Knee cartilage damage can be treated effectively through a variety of treatments, including physical therapy, medications, and surgery. The type of treatment that is recommended will depend on the severity of the damage and the underlying cause of the damage. It is important to work closely with your doctor to determine the best course of treatment for you.