As we age, our joints undergo significant wear and tear, often leading to conditions like knee osteoarthritis and cartilage degeneration. The prospect of regrowing or repairing damaged cartilage has long been a topic of medical research. Recently, infrared therapy has emerged as a promising non-invasive treatment option for knee cartilage repair.
But how does it work? We will explore the mechanisms behind this innovative approach, which involves the use of specific wavelengths of light to stimulate cellular processes and promote tissue repair. By penetrating deep into the tissue, infrared light is believed to enhance healing in damaged cartilage.
This article will provide an overview of the current state of infrared therapy for knee cartilage damage, including its benefits and potential applications for arthritis sufferers.
Key Takeaways
- Infrared therapy is a non-invasive treatment for knee cartilage repair.
- It uses specific light wavelengths to stimulate cellular healing processes.
- This therapy is believed to promote tissue repair in damaged cartilage.
- It may offer benefits for individuals suffering from knee osteoarthritis.
- Infrared therapy could be a potential treatment option for arthritis.
Understanding Knee Cartilage and Osteoarthritis
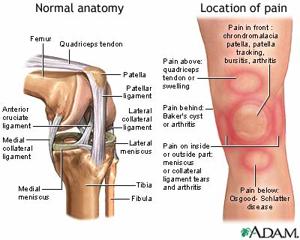
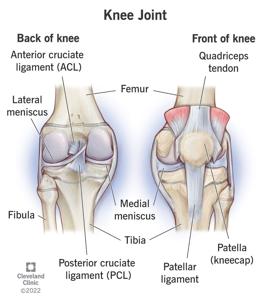
Knee cartilage plays a crucial role in maintaining joint health, and understanding its structure is essential for appreciating the impact of osteoarthritis. The knee joint, one of the body’s largest and most complex joints, is subjected to significant stress and strain throughout our lives.
Articular cartilage, which covers the ends of bones in the knee joint, is composed of highly specialized cells called chondrocytes. These cells are sparsely distributed within the cartilage tissue and have a low replicative ability, which limits the cartilage’s natural repair processes.
The Structure and Function of Knee Cartilage
The complex structure of knee cartilage consists of chondrocytes embedded in an extracellular matrix primarily composed of collagen and proteoglycans. This unique composition allows knee cartilage to provide a smooth, low-friction surface for joint movement while distributing mechanical loads across the joint.
Healthy knee cartilage maintains a delicate balance between the synthesis and degradation of cartilage components. This balance is crucial for maintaining joint integrity and function. However, knee cartilage lacks blood vessels and nerves, significantly limiting its natural ability to repair itself when damaged.
The synovial membrane surrounding the knee joint plays a vital role in nourishing the cartilage and providing lubrication for smooth joint movement through the production of synovial fluid.
| Component | Function | Importance in Knee Cartilage |
|---|---|---|
| Chondrocytes | Specialized cells producing cartilage matrix | Essential for cartilage health and maintenance |
| Collagen | Provides tensile strength to cartilage | Critical for withstanding mechanical stress |
| Proteoglycans | Contributes to cartilage’s compressive stiffness | Vital for load distribution and absorption |
| Synovial Fluid | Lubricates the joint and nourishes cartilage | Essential for smooth joint movement and cartilage health |
Understanding the normal structure and function of knee cartilage provides a foundation for comprehending how osteoarthritis develops and why certain treatments, such as infrared therapy, may be beneficial.
Osteoarthritis is characterized by the degeneration of knee cartilage, leading to joint pain and reduced mobility. Studies have shown that the condition involves a complex interplay of factors, including genetic predisposition, age, and mechanical stress on the joint.
As we explore the relationship between knee cartilage and osteoarthritis, it becomes clear that maintaining healthy cartilage is crucial for preventing or slowing the progression of this debilitating condition.
Understanding Knee Cartilage and Osteoarthritis
Learn Understanding how cartilage degeneration occurs is crucial for developing effective treatments for osteoarthritis and improving patient outcomes. Cartilage degeneration is a complex process influenced by various factors.
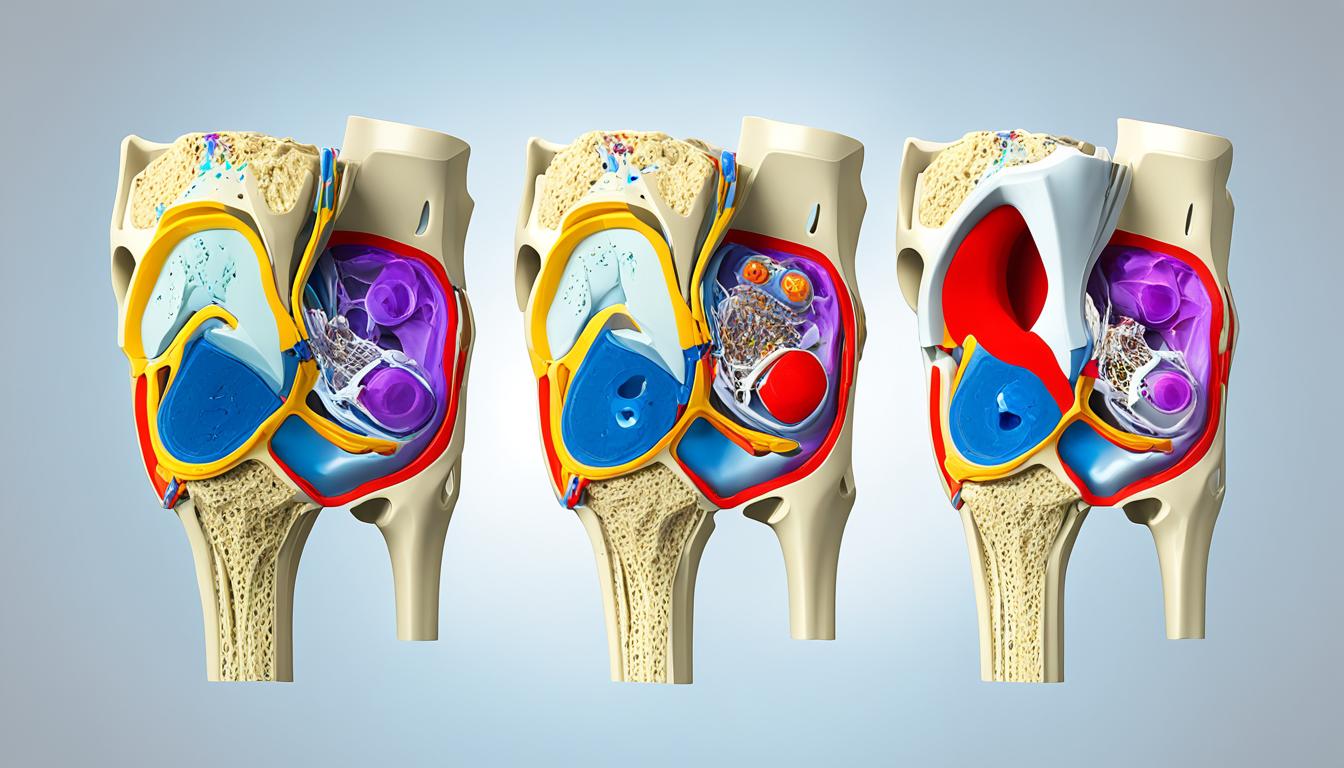
How Cartilage Degeneration Occurs
Cartilage degeneration is characterized by the disruption of the balance between cartilage synthesis and breakdown, leading to progressive joint damage. Osteoarthritis (OA), a degenerative joint disease, is multifactorial in etiology, with age, joint injury, trauma, and obesity being main predisposing risk factors.
The increased expression of inflammation mediators alters cartilage homeostasis by favoring the catabolic activity of chondrocytes, resulting in cartilage matrix disruption and loss. This process is not part of a chronic systemic inflammation but rather a joint-specific mechanism.
Key aspects of cartilage degeneration include:
- The multifactorial nature of cartilage degeneration, including age-related changes and mechanical stress.
- The role of inflammatory mediators in promoting catabolic activity in chondrocytes.
- The process of cartilage matrix disruption and its consequences.
- The progression to joint space narrowing and subchondral bone remodeling.
Understanding these mechanisms is essential for addressing the underlying tissue damage in osteoarthritis and for developing effective treatment strategies.
Understanding Knee Cartilage and Osteoarthritis
Cartilage repair is a complex process, hindered by the avascular nature of cartilage and the limited ability of chondrocytes to proliferate. Articular cartilage is composed of highly specialized cells, chondrocytes, that are sparsely distributed and have low replicative ability. This limited regenerative capacity is a significant challenge in the treatment of cartilage damage.
Challenges in Cartilage Repair
The absence of vascular and neural support in cartilage limits the repair process of damaged cartilage. Traditional healing mechanisms that work for other tissues often fail when it comes to cartilage repair. The complex structure of cartilage makes it difficult to replicate through current tissue engineering approaches.
Conventional treatments for cartilage damage have significant limitations. Medications often only address symptoms rather than promoting actual repair. The “wear and tear” model of osteoarthritis has evolved to include considerations of inflammation and metabolic factors, highlighting the complexity of cartilage degeneration.
Key Challenges in Cartilage Repair:
- Limited proliferative capacity of chondrocytes
- Avascular nature of cartilage
- Complexity of cartilage structure
- Limited effectiveness of conventional treatments
- Evolving understanding of osteoarthritis pathology
Finding effective treatments for cartilage repair has been a persistent challenge in orthopedic medicine. The body’s limited natural response to cartilage damage creates a need for interventions that can stimulate and support the repair process.
| Treatment Challenges | Description | Potential Solution |
|---|---|---|
| Limited Chondrocyte Proliferation | Chondrocytes have low replicative ability | Cellular therapy or growth factor application |
| Avascular Nature | Lack of blood supply hinders repair | Angiogenic therapy or tissue engineering |
| Complex Cartilage Structure | Difficulty in replicating cartilage architecture | Advanced tissue engineering techniques |
The need for effective cartilage repair treatments has driven research into innovative therapies, including infrared therapy. By understanding the challenges in cartilage repair, we can better appreciate the potential benefits of emerging treatments.
What is Infrared Therapy for Knee Cartilage Repair
Infrared therapy has emerged as a promising treatment for knee cartilage repair, leveraging the benefits of photobiomodulation. This non-invasive approach has garnered significant attention in the medical community due to its potential in reducing inflammation and promoting healing.
As we explore the benefits of infrared therapy for knee cartilage, it’s essential to understand the underlying principles of photobiomodulation and how it differs from other light-based treatments. Photobiomodulation therapy involves the use of red or near-infrared light to stimulate cellular processes, reduce inflammation, and relieve pain without causing thermal damage to tissues.
Defining Photobiomodulation and Light Therapy
Photobiomodulation (PBM) is a form of light therapy that has been increasingly recognized for its therapeutic benefits. It encompasses both laser and LED light sources, making it a more inclusive term than the previously used “low-level laser therapy” (LLLT).
The evolution from LLLT to PBM reflects a broader understanding of how different light sources can be utilized for therapeutic purposes. PBM works at the cellular level, promoting beneficial biological responses without causing tissue heating. This is in contrast to other light-based treatments that rely on thermal effects.
One of the key advantages of PBM is its non-invasive nature, making it an attractive option for patients seeking alternatives to surgery or pharmaceutical interventions. As evidence of its efficacy continues to accumulate, PBM is gaining acceptance in mainstream medicine.
The therapeutic use of PBM involves the application of specific wavelengths of light to stimulate healing and reduce inflammation. The effects of PBM on cellular processes are multifaceted, influencing various aspects of tissue repair and regeneration.
| Therapy Type | Light Source | Primary Effects |
|---|---|---|
| Photobiomodulation Therapy | Laser or LED | Reduces inflammation, promotes healing |
| Low-Level Laser Therapy | Laser | Stimulates cellular processes, relieves pain |
| Light Therapy | Various (including LED) | Enhances tissue repair, reduces pain |
By understanding the mechanisms behind PBM and its application in infrared therapy, we can better appreciate its potential benefits for knee cartilage repair. The growing body of research supporting PBM underscores its promise as a valuable treatment option.
What is Infrared Therapy for Knee Cartilage Repair
Infrared therapy devices designed for knee cartilage repair are diverse, including both laser-based and LED-based technologies. This diversity allows for a range of treatment options tailored to specific needs and conditions.
Device Technologies and Form Factors
The devices available for infrared therapy can be broadly categorized into laser-based and LED-based systems. Laser-based devices, including diode lasers, offer precise control over the wavelength and intensity of the light emitted, which can be advantageous for targeting specific tissue depths and conditions.
LED-based systems, on the other hand, utilize light-emitting diodes to produce a broader beam of light, which can be beneficial for treating larger areas. The choice between these technologies depends on the specific requirements of the treatment and the condition being addressed.
Infrared therapy devices also vary significantly in their form factors. Stationary clinical units are typically used in professional settings and offer advanced features and higher power outputs. In contrast, portable handheld devices and wearable pads or wraps are designed for personal use at home, providing convenience and flexibility for ongoing treatment.
Wavelength Specificity and Device Design
The effectiveness of infrared therapy for knee cartilage repair is heavily influenced by the wavelength of the light used. Wavelengths between 632-910 nm are considered particularly effective for promoting cartilage repair. The design of the device, including factors such as power density, beam spot size, and depth of penetration, also plays a crucial role in determining the treatment’s efficacy.
When selecting an infrared therapy device, it’s essential to evaluate its specifications to ensure it meets the requirements for effective knee cartilage treatment. Advances in technology have made infrared therapy more accessible, with increasingly sophisticated yet user-friendly devices becoming available for both clinical and home use.
- Laser-based devices offer precision and control over treatment parameters.
- LED-based systems provide a broader beam of light, suitable for larger treatment areas.
- Device form factors range from stationary clinical units to portable handheld devices and wearable pads or wraps.
- Wavelength specificity is crucial, with 632-910 nm being particularly effective for cartilage repair.
- Device design influences treatment efficacy through factors like power density and depth of penetration.
What is Infrared Therapy for Knee Cartilage Repair
To harness the full potential of infrared therapy for knee cartilage repair, it’s essential to understand the physics behind light penetration into tissue. Infrared therapy, also known as low-level laser therapy (LLLT) or photobiomodulation (PBM), involves the application of infrared light to stimulate cellular processes that can aid in tissue repair.
How Infrared Light Penetrates Tissue
The penetration of infrared light into human tissue is a complex process influenced by several factors, including the wavelength of the light, tissue type, pigmentation, hydration, and the presence of blood vessels. Research indicates that near-infrared light, with wavelengths between 700-1000 nm, generally penetrates deeper into tissue than visible red light.
Factors Affecting Light Penetration
- Tissue type and composition
- Pigmentation and melanin content
- Hydration levels in the tissue
- Presence and density of blood vessels
Understanding these factors is crucial for maximizing the effectiveness of infrared therapy. Proper positioning and application technique are vital to ensure that the infrared light reaches the knee joint effectively.
As infrared light travels through skin, subcutaneous fat, and the joint capsule to reach the cartilage, it interacts with various tissue components. The therapeutic effects of infrared light are not limited to the direct penetration depth, as systemic effects and cellular signaling cascades can extend its benefits beyond the targeted area.
Mechanisms of Action
According to research, photons emitted by PBM are primarily absorbed by cytochrome C oxidase (CCO) within the mitochondrial electron transport chain. This absorption leads to a series of complex cellular responses and altered redox states, which can be explained by two primary redox processes:
| Process | Description | Effect |
|---|---|---|
| Photoexcitation | Photoexcitation of specific chromophores within CCO causes changes in their redox properties. | Speeds up electron transfer |
| Photo-dissociation | CCO releases NO upon photo-dissociation. | Increases oxygen binding and respiration rates |
These mechanisms underscore the potential of infrared therapy to enhance cellular metabolism and promote tissue repair. By understanding how infrared light penetrates tissue and interacts with cellular components, we can better appreciate its therapeutic potential for knee cartilage repair.
The Science Behind Infrared Therapy
By delving into the cellular mechanisms of action, we can better understand how infrared therapy contributes to cartilage health. Infrared therapy, also known as low-level laser therapy (LLLT) or photobiomodulation (PBM), has been shown to have beneficial effects on cells involved in cartilage repair.
Cellular Mechanisms of Action
When cells are exposed to red or near-infrared light, cytochrome c oxidase (CCO) in the mitochondrial respiratory chain absorbs photon energy. This absorption causes an electronic transition, resulting in increased cellular respiration efficiency and ATP synthesis. As a result, PBM can improve cellular metabolism and increase cell membrane potential, contributing to better cellular states such as cell proliferation and normal functional cell activity.
The primary cellular mechanisms through which infrared therapy affects chondrocytes and other cells involved in cartilage repair are multifaceted:
- Cytochrome c oxidase acts as the primary photoacceptor for infrared light, initiating a cascade of cellular responses that lead to increased ATP production.
- The absorption of photons by cytochrome c oxidase enhances cellular energy levels, providing the necessary energy for cellular repair processes.
- Infrared light modulates reactive oxygen species (ROS) levels, with controlled increases in ROS acting as signaling molecules to activate beneficial cellular pathways.
- Infrared therapy influences gene expression in chondrocytes, promoting the synthesis of cartilage matrix components and reducing the expression of degradative enzymes.
Furthermore, infrared therapy affects cell membrane permeability and ion channel activity, influencing cellular signaling and function. These cellular mechanisms collectively contribute to enhanced chondrocyte survival, proliferation, and matrix production, which are essential for cartilage repair.
Studies have shown that the effects of infrared therapy on cells can lead to significant improvements in cartilage health. By understanding the cellular mechanisms of action, we can better appreciate the potential benefits of this therapy for knee cartilage repair.
The Science Behind Infrared Therapy
Infrared therapy has been shown to have a profound impact on cellular function, particularly in the context of mitochondrial activity. Mitochondria are the powerhouses of cells, responsible for producing the energy required for various cellular processes.
Effects on Mitochondria and ATP Production
When cells are exposed to red or near-infrared light, cytochrome c oxidase (CCO) absorbs photon energy, causing an electronic transition from a low-energy level to a high-energy level on the chromophore. This results in the release of an electron that participates in cell respiration and ATP synthesis. As a consequence, photobiomodulation (PBM) can improve cellular respiration efficiency by promoting cellular metabolism and increasing cell membrane potential.
We focus on how infrared therapy specifically targets mitochondria to enhance their function in chondrocytes and surrounding tissues. The process by which infrared light dissociates nitric oxide from cytochrome c oxidase allows for increased oxygen consumption and ATP production. Improved mitochondrial function leads to increased cellular energy availability, which is crucial for cartilage repair processes that require significant metabolic resources.
The relationship between mitochondrial dysfunction in osteoarthritic chondrocytes and the potential for infrared therapy to restore normal function is significant. Enhanced ATP production supports protein synthesis, cell proliferation, and extracellular matrix production in cartilage tissue. Research has demonstrated measurable increases in ATP levels following infrared light exposure, correlating with improved cellular function.
The mitochondrial effects of infrared therapy may help chondrocytes resist the metabolic stress associated with osteoarthritis, potentially slowing disease progression. By enhancing mitochondrial activity, infrared therapy can promote improved cellular function and overall tissue health.
| Cellular Process | Effect of Infrared Therapy | Benefit for Cartilage Repair |
|---|---|---|
| Mitochondrial Function | Enhanced ATP Production | Increased Energy for Cellular Processes |
| Cell Proliferation | Promoted Cell Growth | Improved Tissue Repair |
| Extracellular Matrix Production | Increased Matrix Synthesis | Enhanced Cartilage Health |
Studies have shown that infrared therapy can have a positive impact on various cellular processes, ultimately contributing to improved cartilage health and function. By understanding the effects of infrared therapy on mitochondria and ATP production, we can better appreciate its therapeutic potential for cartilage repair.
The Science Behind Infrared Therapy
Infrared therapy has emerged as a promising treatment for knee cartilage repair, leveraging its anti-inflammatory properties to promote healing. This non-invasive approach has garnered significant attention in recent years due to its potential to modulate the inflammatory response, a key factor in the progression of osteoarthritis and associated pain.
Reduction of Inflammatory Response
Numerous studies have demonstrated the anti-inflammatory effects of Photobiomodulation (PBM), the therapeutic mechanism behind infrared therapy, in the context of arthritis treatment. By regulating various cellular responses, PBM promotes cell activity and functional normalization. This includes enhancing mitochondrial ATP production, releasing intracellular nitric oxide (NO), and modulating the secretion of inflammatory cytokines such as TNFα, IL-6, and IL-β by immune cells.
We will explore how infrared therapy modulates the inflammatory response in osteoarthritic joints. The therapy has been shown to reduce the production of pro-inflammatory cytokines like IL-1β, TNF-α, and IL-6 by affected cells within the joint environment. This reduction is crucial as these cytokines play a significant role in disease progression and pain.
Key Effects of Infrared Therapy on Inflammation:
- Reduces inflammatory cell recruitment and activation, limiting the inflammatory cascade in damaged cartilage.
- Promotes the production of anti-inflammatory cytokines, shifting the balance toward a more regenerative environment.
- Contributes to decreased pain and improved function in patients with knee cartilage damage.
- Affects specific inflammatory signaling pathways, such as NF-κB, which are crucial in osteoarthritis progression.
- Offers potential long-term benefits for cartilage preservation and repair beyond immediate symptomatic relief.
By understanding how infrared therapy impacts the inflammatory response, we can better appreciate its therapeutic potential for managing knee cartilage degeneration and associated conditions like osteoarthritis.
Benefits of Infrared Therapy for Knee Cartilage
Infrared therapy has emerged as a promising treatment for knee cartilage repair by stimulating the synthesis of extracellular matrix components. This non-invasive approach has shown significant potential in promoting the health and repair of knee cartilage.
Stimulation of Extracellular Matrix Synthesis
The extracellular matrix (ECM) is a crucial component of articular cartilage, providing its mechanical properties and playing a vital role in its function. Infrared therapy, particularly low-level laser therapy (LLLT) or photobiomodulation (PBM), has been shown to stimulate chondrocytes to increase their production of ECM components. This includes the synthesis of collagen type II, which is the predominant collagen in healthy articular cartilage, and proteoglycans like aggrecan, which give cartilage its compressive strength and resilience.
Studies have demonstrated that infrared light can activate growth factors that promote matrix synthesis, such as transforming growth factor-beta (TGF-β) and insulin-like growth factor-1 (IGF-1). These growth factors play a crucial role in regulating the metabolic activity of chondrocytes and enhancing the production of ECM components.
The increased matrix synthesis contributes to the structural integrity of damaged cartilage and may help fill in defects or areas of thinning. Research evidence from both laboratory and clinical studies has demonstrated enhanced matrix production in response to specific infrared therapy protocols.
- Infrared therapy stimulates chondrocytes to produce more ECM components, essential for cartilage repair.
- The therapy enhances the production of collagen type II and proteoglycans, critical for maintaining healthy articular cartilage.
- Growth factors such as TGF-β and IGF-1 are activated by infrared light, promoting matrix synthesis.
- Increased matrix synthesis helps restore the structural integrity of damaged cartilage.
- Clinical and laboratory studies support the effectiveness of infrared therapy in enhancing matrix production.
By understanding how infrared therapy stimulates ECM synthesis, we can better appreciate its potential benefits for knee cartilage repair. As research continues to uncover the mechanisms behind this therapy, it is likely that infrared therapy will become an increasingly important tool in the treatment of cartilage-related disorders.
Benefits of Infrared Therapy for Knee Cartilage
Infrared therapy has emerged as a promising treatment for reducing cartilage degradation in knee osteoarthritis patients. This therapeutic approach leverages the benefits of infrared light to create a favorable environment for cartilage health.
Reduction of Cartilage Degradation
One of the key benefits of infrared therapy is its ability to reduce cartilage degradation. Cartilage degradation is a significant concern in osteoarthritis, as it leads to the loss of joint function and increased pain. Infrared therapy helps by inhibiting the activity of destructive enzymes in the joint environment. These enzymes, including matrix metalloproteinases (MMPs) and aggrecanases, play a crucial role in breaking down cartilage components.
Studies have shown that infrared light decreases the expression and activity of these enzymes, thereby reducing the rate of cartilage degradation. Additionally, infrared therapy has been found to reduce oxidative stress in the joint, which is a contributing factor to cartilage matrix degradation.
Preserving chondrocyte viability is essential for maintaining healthy cartilage. Infrared therapy has been shown to support the health of these cells, thereby preventing further cartilage loss. Furthermore, infrared therapy may help stabilize the cartilage matrix by promoting the cross-linking of collagen fibers and other structural components.
The combined effect of reduced cartilage degradation and enhanced matrix synthesis creates a net positive impact on cartilage health. Clinical and experimental evidence supports the notion that infrared therapy can lead to reduced rates of cartilage loss in subjects receiving treatment compared to control groups.
- Infrared therapy inhibits destructive enzymes in the joint, reducing cartilage breakdown.
- It decreases the expression and activity of MMPs and aggrecanases, key enzymes involved in cartilage degradation.
- Infrared therapy reduces oxidative stress, a factor contributing to cartilage matrix degradation.
- It preserves chondrocyte viability, essential for maintaining healthy cartilage.
- Infrared therapy may stabilize the cartilage matrix by promoting cross-linking of collagen fibers.
By understanding the mechanisms through which infrared therapy acts, we can better appreciate its potential as a therapeutic option for individuals with knee osteoarthritis. The evidence suggests that infrared therapy can be a valuable adjunct in the management of cartilage health.
Benefits of Infrared Therapy for Knee Cartilage
Infrared therapy has emerged as a promising treatment for knee cartilage damage and osteoarthritis, offering significant pain relief and improved mobility. This non-invasive approach has garnered attention for its potential to address the underlying causes of pain and limited mobility in patients with knee osteoarthritis.
Pain Relief and Improved Mobility
One of the primary benefits of infrared therapy is its ability to provide pain relief for patients suffering from knee cartilage damage and osteoarthritis. We will explore the mechanisms through which infrared therapy achieves this, including its effects on nerve conduction and the release of pain mediators in the joint.
Studies have shown that infrared therapy can lead to significant reductions in pain-like behavior in animal models. While there were conflicting findings regarding some biochemical, histological, and behavioral outcomes, the overall trend suggests that infrared therapy can be an effective treatment for pain management.
The relationship between reduced inflammation and decreased pain is a crucial aspect of infrared therapy’s benefits. By mitigating inflammation, infrared therapy can lead to improved comfort and reduced pain for patients. This, in turn, contributes to improved mobility, creating a positive cycle where increased movement further benefits joint health.
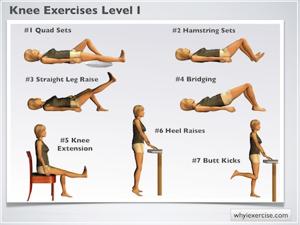
Improved mobility following infrared therapy can also help patients engage more effectively in physical therapy and exercise programs. This is a critical component of comprehensive care for knee osteoarthritis, as increased mobility and strength can lead to better overall outcomes.
Clinical evidence supports the use of infrared therapy for pain reduction and functional improvement in patients with knee cartilage issues. Randomized controlled trials have demonstrated the efficacy of this treatment approach, providing a solid foundation for its inclusion in treatment protocols.
- Infrared therapy provides pain relief by affecting nerve conduction and the release of pain mediators.
- The anti-inflammatory effects of infrared therapy contribute to decreased pain and improved comfort.
- Pain relief and improved mobility create a positive cycle, enhancing overall joint health.
Clinical Evidence Supporting Infrared Therapy
In vitro studies on chondrocytes provide valuable insights into the cellular mechanisms underlying infrared therapy’s effects on knee cartilage. These controlled laboratory experiments help us understand how infrared light interacts with the cells responsible for maintaining cartilage health.
In Vitro Studies on Chondrocytes
Several in vitro studies have investigated the effects of infrared therapy on chondrocytes, the specialized cells found in healthy cartilage. These studies used monocultures experiments, where chondrocytes were isolated and cultured in controlled laboratory conditions.
Two-thirds of the studies used chondrocytes isolated from the knee cartilage of New Zealand white rabbits, which were further expanded in vitro. The remaining study used human chondrocytes cell lines. This diversity in cell sources helps to establish the broader applicability of the findings.
One-third of the studies conducted experiments in an in vitro OA model, which involved administering recombinant human interleukin-1β (IL-1β) to stimulate the inflammatory environment characteristic of osteoarthritic knees. This approach allowed researchers to examine how infrared therapy modifies cellular responses under conditions that mimic osteoarthritis.
The studies examined various aspects of chondrocyte behavior, including proliferation, survival, and metabolic activity. They also investigated how infrared light affects chondrocyte gene expression, particularly genes related to matrix production and inflammatory mediators.
The results of these studies are summarized in the following table:
| Study | Cell Source | Experimental Model | Key Findings |
|---|---|---|---|
| Study 1 | Rabbit chondrocytes | Normal | Enhanced cell proliferation and matrix production |
| Study 2 | Human chondrocytes | OA model (IL-1β) | Reduced inflammatory responses and increased cartilage-specific gene expression |
| Study 3 | Rabbit chondrocytes | Normal | Improved cell survival and metabolic activity |
These in vitro studies provide valuable insights into the potential benefits of infrared therapy for knee cartilage repair. While they have limitations, they contribute significantly to our understanding of the cellular mechanisms underlying the therapy’s effects.
Clinical Evidence Supporting Infrared Therapy

Animal studies have played a crucial role in understanding how infrared therapy influences cartilage health in models of osteoarthritis and joint damage. These studies have provided valuable insights into the potential therapeutic benefits of infrared therapy for knee cartilage repair.
Animal Model Research Results
Various animal models have been used to study infrared therapy, including surgically-induced osteoarthritis, chemical induction models, and traumatic injury models. These models have allowed researchers to investigate the effects of infrared therapy on cartilage repair and regeneration in a controlled manner.
Histological Evidence
Histological examinations from animal studies have shown significant improvements in cartilage structure, thickness, and quality following infrared therapy. These improvements suggest that infrared therapy can stimulate cartilage repair and potentially slow down or halt the progression of osteoarthritis.
Biochemical Changes
The biochemical changes observed in animal cartilage after infrared treatment have been explored, including alterations in inflammatory markers and cartilage-specific molecules. These changes indicate a reduction in inflammation and an increase in cartilage health.
Behavioral Outcomes
Animal studies have also highlighted improvements in weight-bearing, mobility, and pain-related behaviors following infrared therapy. These outcomes suggest that infrared therapy can improve the quality of life for subjects with osteoarthritis or joint injuries.
The methodological quality of these animal studies was assessed using the Risk of Bias Assessment tool for Non-Randomized Studies (RoBANS), which evaluates the risk of bias across six domains. This assessment is crucial for understanding the reliability of the findings and their potential applicability to human patients.
By examining the results from animal model research, we can better understand the potential benefits and limitations of infrared therapy for knee cartilage repair. This knowledge can inform the development of effective treatment protocols for human patients.
Clinical Evidence Supporting Infrared Therapy
Infrared therapy has garnered significant attention in recent years due to its potential in treating knee osteoarthritis and promoting cartilage repair. Human clinical trials have been instrumental in understanding the efficacy of this treatment modality.
Outcomes from Human Clinical Trials
Numerous studies have investigated the effects of infrared therapy on knee cartilage repair and osteoarthritis treatment. These trials have employed various strategies and laser therapy (LT) parameters, resulting in positive effects on cartilage repair. The evidence suggests that LT may be an adequate therapy for osteoarthritis (OA) treatment.
We examined the results of human clinical trials that evaluated infrared therapy for knee cartilage repair and osteoarthritis treatment. Both randomized controlled trials and observational studies provided evidence for infrared therapy’s effectiveness in real-world clinical settings.
The studies measured objective outcomes such as changes in cartilage volume, joint space width, and inflammatory markers following infrared therapy. Patient-reported outcomes from clinical trials were also significant, highlighting improvements in pain scores, functional assessments, and quality of life measures.
Comparison of Treatment Outcomes
| Treatment Modality | Pain Reduction | Cartilage Repair | Functional Improvement |
|---|---|---|---|
| Infrared Therapy | Significant | Moderate | Significant |
| Standard Treatment | Moderate | Minimal | Moderate |
The durability of treatment effects observed in longer-term follow-up studies was also a crucial aspect. Improvements were generally maintained over time, indicating the potential long-term benefits of infrared therapy.
In conclusion, human clinical trials have provided substantial evidence supporting the use of infrared therapy for knee cartilage repair and osteoarthritis treatment. The positive outcomes observed in these studies underscore the potential of infrared therapy as a valuable treatment option.
Preparing for Infrared Therapy Treatment
When considering infrared therapy for knee cartilage repair, it’s crucial to assess whether you’re a suitable candidate for this treatment. Infrared therapy has shown promise in treating knee osteoarthritis and cartilage damage, but its effectiveness can vary based on several factors.
Candidacy Factors for Infrared Therapy
Several key factors determine whether a patient is a good candidate for infrared therapy. These include the severity and type of cartilage damage, the patient’s overall health status, and their previous treatments.
The severity of knee osteoarthritis or cartilage damage plays a significant role in determining the potential effectiveness of infrared therapy. Patients with mild to moderate cartilage damage tend to respond better to this treatment than those with severe degeneration.
| Factor | Influence on Candidacy |
|---|---|
| Severity of Cartilage Damage | Mild to moderate damage responds better |
| Type of Cartilage Damage | Traumatic injuries may respond differently than degenerative conditions |
| Patient Age | Older patients may have reduced responsiveness |
| Overall Health Status | Presence of comorbidities can affect treatment outcomes |
Patient factors such as age, overall health status, and activity level also play a crucial role in determining candidacy. Older patients or those with significant comorbidities may have a reduced response to infrared therapy.
Previous treatments and their outcomes can also influence candidacy for infrared therapy. Patients who have not responded to other conservative treatments may still benefit from infrared therapy.
It’s essential to understand that infrared therapy is not suitable for everyone. Certain medical conditions and medications may contraindicate this treatment. A thorough assessment by a healthcare provider is necessary to determine suitability.
Ultimately, determining candidacy for infrared therapy involves a shared decision-making process between patients and healthcare providers. By carefully evaluating individual factors and setting realistic expectations, patients can make informed decisions about whether infrared therapy is right for them.
Preparing for Infrared Therapy Treatment
Before starting infrared therapy, it’s essential for patients to understand what this treatment can achieve for their knee cartilage health. Infrared therapy has shown promise in reducing pain and improving cartilage health in patients with knee osteoarthritis.
Factors Influencing Treatment Outcomes
The effects of infrared therapy can vary among patients. Several factors influence the outcomes, including the severity of knee osteoarthritis, the patient’s overall health, and how well they adhere to the treatment plan. Studies have shown that patients with mild to moderate knee osteoarthritis tend to respond better to infrared therapy than those with severe cartilage degeneration.
When considering infrared therapy, patients should be aware of the typical timeline for experiencing benefits. Some may notice initial pain relief within a few sessions, while longer-term cartilage improvements may take several weeks to become apparent. It’s also important to understand that infrared therapy is often most effective as part of a multimodal treatment approach, combining it with other therapies such as physical therapy and nutritional support.
The limitations of infrared therapy should also be considered. Patients with severe cartilage damage or certain other health conditions may not respond as well to this treatment. We will help patients develop realistic expectations about what infrared therapy can achieve based on current scientific evidence and individual assessments.
To evaluate progress during treatment, patients should look for improvements in pain levels, mobility, and overall knee function. Regular assessments will help determine the effectiveness of the treatment and guide any necessary adjustments to the treatment plan.
In conclusion, setting realistic expectations is crucial for patients undergoing infrared therapy for knee cartilage repair. By understanding the potential benefits, limitations, and factors influencing treatment outcomes, patients can make informed decisions about their care.
Step-by-Step Infrared Therapy Protocol
Before starting infrared therapy for knee cartilage repair, several preparations are necessary to ensure effective treatment. Proper preparation can significantly impact the outcome of the therapy.
Pre-Treatment Preparations
To ensure the effectiveness of infrared therapy, several pre-treatment preparations are necessary. Proper skin preparation is crucial, involving thorough cleaning of the treatment area and removal of any substances that might block light penetration, such as lotions or oils.
Patients should also be aware of any activity restrictions or dietary considerations that may be recommended before infrared therapy sessions. For instance, avoiding strenuous activities or certain foods might be advised to optimize the treatment effects.
The attire worn during treatment sessions should provide easy access to the knee while maintaining comfort and dignity. Loose, comfortable clothing is typically recommended to facilitate the treatment process.
Hydration is another important factor; patients are usually advised to be well-hydrated before treatment as it may influence the effectiveness of infrared therapy. Adequate hydration can enhance the body’s response to the treatment.
Timing infrared therapy in relation to other treatments or medications is also critical. Patients should consult with their healthcare provider to determine the optimal schedule for their infrared therapy sessions.
A pre-treatment assessment should occur at each session, including baseline measurements of pain, range of motion, and other relevant parameters. This helps in tracking progress and adjusting the treatment protocol as necessary.
As noted in a study on the effects of low-level laser therapy, “The therapeutic effects of laser therapy are based on the absorption of light by cellular chromophores, leading to various biological responses.” This underscores the importance of proper preparation to ensure effective light absorption.
Step-by-Step Infrared Therapy Protocol
Infrared therapy has emerged as a promising treatment for knee cartilage repair, offering a non-invasive approach to stimulate healing and reduce pain. As we delve into the step-by-step protocol for this therapy, it’s essential to understand the critical role of proper positioning in ensuring the effectiveness of the treatment.
Positioning for Optimal Light Exposure
Achieving the right position during infrared therapy is essential for ensuring that the light penetrates effectively to the targeted knee cartilage area. The positioning can significantly affect the therapy’s efficacy, as it influences how deeply the infrared light can penetrate the tissue.
When using infrared laser therapy for knee cartilage repair, the position of the knee and the surrounding tissue can impact the treatment’s success. For instance, the angle of the joint and the compression of the tissue can either facilitate or hinder the penetration of the infrared light. Therefore, it’s crucial to position the knee in a way that maximizes exposure to the infrared light.
Positioning Options for Different Devices
Different infrared therapy devices may require different positioning strategies. For example, stationary clinical units might necessitate a more standardized positioning approach, whereas portable home devices offer more flexibility in terms of patient positioning.
- For stationary clinical units, patients may need to adjust their position to align the affected area with the device’s applicator.
- Portable devices allow patients to position themselves comfortably while ensuring the device is correctly aligned with the treatment area.
As noted by experts, “The effectiveness of low-level laser therapy (LLLT) or photobiomodulation (PBM) is highly dependent on the correct application technique, including proper positioning of the device relative to the target tissue.”
This emphasizes the need for clear guidance on positioning to achieve optimal results from infrared therapy.
To achieve optimal light exposure, patients should be aware of the following factors:
| Factor | Description | Impact on Therapy |
|---|---|---|
| Joint Angle | The degree to which the knee is bent or straightened. | Affects the depth of light penetration. |
| Tissue Compression | The amount of pressure on the tissue surrounding the knee. | Influences the scattering of light within the tissue. |
| Device Alignment | The positioning of the infrared device relative to the knee. | Critical for ensuring the light is delivered to the targeted area. |
By understanding and adjusting these factors, patients and practitioners can work together to achieve the most effective treatment outcomes. Studies have shown that when properly positioned, infrared therapy can lead to significant improvements in knee cartilage health and function.
Step-by-Step Infrared Therapy Protocol
To achieve the best results from infrared therapy for knee cartilage repair, it’s essential to carefully consider both the length and frequency of treatment sessions. The therapeutic effects of infrared therapy are well-documented, but optimal outcomes depend on a well-structured treatment plan.
Treatment Duration and Frequency
The duration and frequency of infrared therapy sessions can significantly impact their effectiveness. Studies have reported varying parameters for successful treatment outcomes.
All studies analyzed provided detailed information on treatment parameters, including wavelength, operating mode, power output, energy density, irradiation time, treatment duration, and irradiation area. The median laser wavelength used was 632.8 nm, with a range of 632.8-910.0 nm. The median power output was 7 mW, ranging from 2.5 to 10.0 mW, and the median energy density was 4.0 J/cm², with a range of 2.50-5.87 J/cm². Treatment durations varied, with a median of 390 seconds (range, 180-660 seconds) and a median irradiating area of 0.91 cm² (range, 0.785-9.6 cm²).
The light stimulus was administered in pulse mode in one study (33%) and in continuous mode in the remaining two studies (67%). These variations highlight the need for personalized treatment protocols.
Key Considerations for Treatment Duration and Frequency:
- Typical session lengths can range from a few minutes to longer treatments, depending on the power density and wavelength of the infrared device.
- The frequency of treatments can vary, with daily sessions often recommended during intensive treatment phases, tapering to maintenance protocols once improvements are established.
- Treatment dosage, calculated as energy density (J/cm²), is critical for treatment planning and effectiveness.
- Protocols may evolve over time as the patient responds to therapy, potentially transitioning from more frequent to less frequent sessions.
- Clinical evidence suggests that the total number of treatment sessions required can vary, but there is a point at which additional treatments may no longer provide significant incremental benefits.
Understanding these factors is crucial for both practitioners and patients to make informed decisions about continuing therapy and to optimize treatment outcomes.
Step-by-Step Infrared Therapy Protocol
To achieve optimal results from infrared therapy, it’s essential to follow a recommended post-treatment care regimen. Proper care after treatment can significantly enhance the effectiveness of the therapy for knee cartilage repair.
Care After Treatment
After undergoing infrared therapy, patients should be aware of the necessary steps to maximize the benefits and minimize any potential adverse effects. This includes understanding any activity restrictions and how soon normal activities can be resumed.
Generally, patients can resume their normal activities shortly after treatment, but it’s advisable to avoid strenuous exercises or heavy lifting for a few hours. Gentle stretching and specific exercises can be beneficial when recommended by a healthcare professional.
Staying hydrated is also crucial following infrared therapy. Hydration supports the cellular processes activated by the treatment, aiding in the repair of knee cartilage. Drinking plenty of water is recommended.
Some patients may experience mild soreness or increased sensitivity in the treated area. Monitoring and managing these temporary responses is essential. Over-the-counter pain relievers or topical creams may be recommended, but always under the guidance of a healthcare provider.
Infrared therapy can be integrated with other treatment modalities, such as physical therapy or exercise programs. The timing and potential interactions should be discussed with a healthcare professional to ensure a cohesive treatment plan.
Tracking Progress
Patients can track their progress between sessions by assessing pain levels, knee function, and other relevant outcomes. Keeping a journal or using a mobile app can be helpful.
| Assessment Criteria | Pre-Treatment | Post-Treatment |
|---|---|---|
| Pain Level (1-10) | 8 | 4 |
| Knee Flexibility (degrees) | 90 | 120 |
| Ability to Perform Daily Activities | Limited | Improved |
By following these post-treatment care guidelines and working closely with a healthcare provider, patients can optimize the benefits of infrared therapy for knee cartilage repair.
Optimal Parameters for Knee Cartilage Repair
Infrared therapy has emerged as a promising treatment for knee cartilage repair, with wavelength selection being a critical factor in its success. The range of 632-910 nm has been identified as particularly effective for this application.
Wavelength Selection (632-910 nm)
The wavelength of infrared light used in therapy plays a pivotal role in determining its effectiveness for knee cartilage repair. Different wavelengths within the 632-910 nm range interact with biological tissues in distinct ways, influencing the therapeutic outcomes. Studies have shown that wavelengths between 632.8 nm and 910.0 nm can significantly impact cartilage repair.
When selecting a wavelength, it’s essential to consider how different wavelengths penetrate tissue and affect cellular processes. For instance, longer wavelengths (800-900 nm) are preferred for reaching deeper knee cartilage structures due to their deeper penetration depth.
The specific cellular responses to different wavelengths are also crucial. Various chromophores (light-absorbing molecules) are activated at different points in the spectrum, influencing the therapeutic effects. Research evidence comparing outcomes with different wavelengths helps guide the selection of the most appropriate light source for specific cartilage conditions.
For example, a median laser wavelength of 632.8 nm has been used in studies, with a range of 632.8-910.0 nm, alongside a median power output of 7 mW and a median energy density of 4.0 J/cm2. These parameters have been associated with positive outcomes in cartilage repair.
As we consider the practical implications of wavelength selection, it becomes clear that individual patient factors such as tissue thickness, skin pigmentation, and the specific location of cartilage damage must be taken into account. This personalized approach ensures that the chosen wavelength is optimal for the patient’s condition.
“The optimal wavelength for infrared therapy can vary based on the specific condition being treated and the individual patient’s characteristics,” as noted in recent studies. This underscores the importance of a tailored approach to wavelength selection.
In conclusion, the selection of the appropriate wavelength within the 632-910 nm range is a critical factor in the effectiveness of infrared therapy for knee cartilage repair. By understanding how different wavelengths interact with biological tissues and influence cellular processes, healthcare providers can optimize treatment outcomes for their patients.
Optimal Parameters for Knee Cartilage Repair
Effective infrared therapy for knee cartilage repair requires a deep understanding of the therapeutic window defined by power density and energy dosage. These parameters are crucial in ensuring that the treatment is both safe and effective.
Power Density and Energy Dosage
Power density, also known as irradiance, and energy dosage, or fluence, are fundamental parameters in low-level laser therapy. Power density refers to the intensity of the laser light applied to the treatment area, typically measured in milliwatts per square centimeter (mW/cm²). Energy dosage, on the other hand, represents the total energy delivered per unit area, usually expressed in joules per square centimeter (J/cm²).
The median laser wavelength used in studies was 632.8 nm, with a range of 632.8-910.0 nm. The median power output was 7 mW, ranging from 2.5 to 10.0 mW. The median energy density was 4.0 J/cm², with a range of 2.50-5.87 J/cm², applied for a median duration of 390 seconds (range, 180-660 seconds) over a median irradiating area of 0.91 cm² (range, 0.785-9.6 cm²).
| Parameter | Median Value | Range |
|---|---|---|
| Laser Wavelength (nm) | 632.8 | 632.8-910.0 |
| Power Output (mW) | 7 | 2.5-10.0 |
| Energy Density (J/cm²) | 4.0 | 2.50-5.87 |
| Treatment Duration (seconds) | 390 | 180-660 |
| Irradiating Area (cm²) | 0.91 | 0.785-9.6 |
The therapeutic window concept is critical in low-level laser therapy. Too little energy may result in ineffective treatment, while too much energy can inhibit beneficial responses or even cause tissue damage. The interaction between power density and treatment time is also significant; longer treatments with lower power may produce different effects than shorter treatments with higher power.
Adjusting power density and energy dosage based on specific treatment goals, such as pain relief versus cartilage regeneration, is essential. For pain relief, a different set of parameters might be more effective compared to promoting cartilage regeneration.
Ensuring consistent and appropriate dosing across treatment sessions is crucial for both practitioners and patients. This involves understanding device specifications and treatment protocols to achieve optimal outcomes.
In conclusion, the optimal parameters for knee cartilage repair using infrared therapy involve a careful balance of power density and energy dosage. By understanding these parameters and how they interact with treatment time and goals, practitioners can provide more effective treatments.
Optimal Parameters for Knee Cartilage Repair
The delivery method of infrared light, whether continuous or pulsed, plays a significant role in its efficacy for cartilage repair. Infrared therapy, also known as low-level laser therapy, has been explored for its potential in promoting knee cartilage health.
Delivery Modes for Infrared Light Therapy
Infrared light can be applied in two primary modes: continuous and pulsed. Continuous mode involves the constant emission of light, while pulsed mode delivers light in intermittent pulses. The choice between these modes can significantly affect treatment outcomes.
Research indicates that the light stimulus was used in pulse mode in 33% of studies and continuously in 67%. This variation in application methods suggests that both approaches have been explored for their therapeutic potential.
Theoretical advantages of pulsed mode include the potential for deeper tissue penetration and the prevention of thermal buildup. Different pulse frequencies may influence biological responses in cartilage and surrounding tissues, offering a nuanced approach to treatment.
| Mode | Characteristics | Theoretical Advantages |
|---|---|---|
| Continuous | Constant emission of light | Simplified treatment protocol |
| Pulsed | Intermittent pulses of light | Deeper penetration, reduced thermal buildup |
The duty cycle, or the proportion of time the light is on during pulsed treatments, affects overall energy delivery and treatment outcomes. Practitioners must consider these factors when selecting the appropriate mode based on individual patient needs and treatment goals.
By understanding the differences between continuous and pulsed mode applications, healthcare providers can optimize infrared therapy protocols for knee cartilage repair. Our analysis of various studies highlights the importance of tailoring treatment parameters to achieve the best possible outcomes.
Professional vs. At-Home Infrared Therapy
For those seeking infrared therapy for knee cartilage repair, understanding the distinctions between professional and at-home treatments is essential. The decision between these two options can significantly impact the effectiveness of the treatment.
Clinical-Grade Equipment Benefits
Professional infrared therapy utilizes clinical-grade equipment that offers several advantages over consumer devices available for at-home use.
The superior specifications of professional equipment include more precise wavelength control, higher power capabilities, and better beam quality. These factors contribute to more effective treatment outcomes.
One of the key benefits of professional equipment is the ability to customize treatment parameters. This allows healthcare providers to tailor the therapy to individual patient needs, potentially leading to more effective cartilage repair.
Key Features of Clinical-Grade Equipment:
- Precise wavelength control (typically in the 632-910 nm range)
- Higher power capabilities for deeper tissue penetration
- Better beam quality for more accurate targeting
- Multiple treatment parameter options for customized protocols
Professional administration by trained healthcare providers also plays a crucial role in the effectiveness of infrared therapy. Proper positioning, accurate targeting, and ongoing assessment are all critical components of successful treatment.
In a clinical setting, infrared therapy is often combined with complementary treatments and expert guidance, providing a comprehensive approach to addressing knee cartilage issues. This integrated approach can lead to more comprehensive care and potentially better outcomes for patients.
| Feature | Professional Infrared Therapy | At-Home Infrared Therapy |
|---|---|---|
| Equipment Quality | Clinical-grade, high-precision devices | Consumer-grade devices with variable quality |
| Customization | Tailored treatment protocols based on individual patient needs | Limited customization options |
| Administration | Performed by trained healthcare professionals | Self-administered by patients |
While at-home infrared therapy devices are available and may offer convenience and cost savings, the benefits of professional treatment should be carefully considered. The advanced equipment, expert administration, and comprehensive care provided in a clinical setting can potentially lead to more effective treatment outcomes.
As research in this field continues to evolve, it’s essential for patients to consult with healthcare professionals to determine the most appropriate treatment plan for their specific needs.
Professional vs. At-Home Infrared Therapy
When considering at-home infrared therapy for knee cartilage repair, it’s crucial to understand what makes a device effective. As we navigate the options available for home use, several factors come into play to ensure we’re using a device that can provide the desired therapeutic effects.
Consumer Devices: What to Look For
When evaluating consumer infrared therapy devices for home use in treating knee cartilage problems, there are several key specifications to consider. The wavelength range of the device is critical, as it determines the depth of penetration and the type of tissue that can be treated effectively. Devices emitting light in the 630-910 nm range are often considered optimal for various therapeutic applications, including knee cartilage repair.
Another important factor is the power output of the device, which affects the treatment duration and intensity. A device with adjustable power settings can be beneficial, allowing users to customize their treatment based on comfort and therapeutic needs. The treatment area coverage is also a significant consideration, as larger treatment areas may be more convenient but could potentially be less intense if the power is not adequately concentrated.
Infrared therapy devices for home use come in various form factors, each with its advantages and limitations. Handheld wands offer flexibility and precision, allowing users to target specific areas. Wearable wraps can provide consistent coverage over a larger area and may be more convenient for some users. Stationary units can offer a more controlled treatment environment but may be less portable.
The importance of FDA clearance or other regulatory approvals cannot be overstated, as these serve as indicators of the device’s safety and manufacturing quality. When evaluating devices, we should also consider the manufacturer’s reputation, warranty offerings, and customer support, as these factors can significantly impact the overall user experience and device reliability.
Pricing for effective home devices can vary widely, and it’s essential to be aware of reasonable price ranges while being cautious of products making exaggerated or unsupported claims. When comparing devices, factors such as ease of use, battery life or power requirements, and durability should be taken into account to ensure the device meets our needs and provides a satisfactory user experience.
- Look for devices with adjustable power settings to customize treatment intensity and duration.
- Consider the treatment area coverage and whether it meets your specific needs.
- Check for FDA clearance or other regulatory approvals as a mark of safety and quality.
- Evaluate the manufacturer’s reputation and customer support offerings.
- Be cautious of devices making unsubstantiated claims about their therapeutic effects.
Professional vs. At-Home Infrared Therapy
As more patients turn to self-administered infrared therapy, understanding the safety considerations becomes crucial. While infrared therapy can be an effective treatment for knee cartilage repair, it’s essential to be aware of the potential risks and take necessary precautions.
Safety Considerations for Self-Administration
When using infrared therapy devices at home, eye protection is paramount. Devices emitting laser light, in particular, require careful handling to avoid accidental exposure to the eyes. We recommend always wearing appropriate eye protection when administering treatment.
To avoid potential skin reactions or burns, it’s crucial to follow the recommended treatment durations and keep the device in motion when appropriate. Static application of the device to a single area for too long can increase the risk of adverse effects.
Following the manufacturer’s instructions regarding treatment frequency and duration is vital to prevent overtreatment. Overuse of infrared therapy can lead to unwanted effects, negating the benefits of the treatment.
Certain individuals should exercise caution or avoid self-administered infrared therapy altogether. Contraindications include certain skin conditions, photosensitivity, and active cancer in the treatment area. It’s essential to consult with a healthcare professional before starting treatment if you have any underlying medical conditions.
Being able to recognize adverse reactions is crucial. If you experience any unusual symptoms such as increased pain, redness, or swelling, discontinue treatment and seek medical advice.
Proper maintenance of the infrared therapy device is also important. Regularly clean the device according to the manufacturer’s instructions and check for any damaged components that could affect safety or efficacy.
| Safety Consideration | Precaution | Benefit |
|---|---|---|
| Eye Protection | Wear appropriate eye protection | Prevents eye damage from laser exposure |
| Skin Reactions | Follow treatment guidelines and keep device in motion | Reduces risk of burns or irritation |
| Treatment Frequency | Adhere to manufacturer’s instructions | Prevents overtreatment and adverse effects |
By being aware of these safety considerations and taking the necessary precautions, patients can safely and effectively use infrared therapy at home for knee cartilage repair.
Combining Infrared Therapy with Other Treatments
Infrared therapy is most effective when combined with other evidence-based treatments for knee cartilage health. By integrating infrared therapy with other therapeutic approaches, healthcare providers can create a comprehensive treatment plan that addresses multiple aspects of knee cartilage repair.
Physical Therapy and Exercise Programs
One of the most effective ways to enhance the benefits of infrared therapy is by combining it with physical therapy and targeted exercise programs. Physical therapy can help improve joint mobility and strengthen the surrounding muscles, which in turn can enhance the effectiveness of infrared therapy. Studies have shown that patients who undergo a combination of infrared therapy and physical therapy experience significant improvements in pain reduction and functional ability.
Infrared therapy can prepare the joint for more effective physical therapy by reducing pain and inflammation before exercise. This can be particularly beneficial for patients with knee cartilage damage, as it allows them to participate more comfortably in physical therapy sessions. As noted by a study published in a reputable medical journal, “The application of infrared therapy prior to exercise can significantly reduce pain and improve functional outcomes in patients with knee osteoarthritis.”
“The combination of infrared therapy and exercise has been shown to promote cartilage health and improve joint function in patients with knee osteoarthritis.”
Specific exercise types that complement infrared therapy for cartilage health include low-impact aerobic activities, appropriate strength training, and range-of-motion exercises. For example, exercises such as cycling, swimming, and gentle stretching can help improve joint mobility without putting excessive stress on the knee joint.
The optimal timing and sequencing of infrared therapy in relation to exercise sessions can vary depending on the individual patient’s needs and response to treatment. However, research suggests that applying infrared therapy before exercise can be particularly effective in reducing pain and improving functional outcomes.
Physical therapists and other practitioners can collaborate to create comprehensive treatment plans that incorporate both infrared therapy and appropriate exercise. By working together, healthcare providers can ensure that patients receive a well-rounded treatment program that addresses their specific needs and promotes optimal outcomes.
- Combining infrared therapy with physical therapy and exercise programs can create synergistic benefits for knee cartilage repair.
- Infrared therapy can reduce pain and inflammation, making it easier for patients to participate in physical therapy and exercise.
- A comprehensive treatment plan that includes infrared therapy, physical therapy, and exercise can lead to improved outcomes for patients with knee cartilage damage.
Combining Infrared Therapy with Other Treatments
As we explore the multifaceted approach to knee cartilage repair, it becomes evident that nutritional support plays a crucial role in complementing infrared therapy. The synergy between these two approaches can potentially enhance the overall effectiveness of the treatment.
Nutritional Support for Cartilage Health
Nutritional support is essential for maintaining healthy cartilage and facilitating its repair. Certain nutrients have been identified as particularly beneficial for cartilage health, including glucosamine and chondroitin, which are naturally occurring compounds found in the body.
Glucosamine and chondroitin are key components of the cartilage matrix, and supplementing with these nutrients may help support cartilage health and potentially slow down its degeneration. Collagen peptides are another important nutrient that can aid in cartilage repair by providing essential amino acids for collagen synthesis.
In addition to these specific supplements, a balanced diet rich in essential vitamins and minerals is crucial for overall cartilage health. Vitamin D and magnesium are examples of nutrients that play important roles in maintaining healthy joints.
Anti-inflammatory foods and supplements can also work synergistically with infrared therapy to reduce joint inflammation. Foods rich in omega-3 fatty acids, such as fatty fish, and certain spices like turmeric, which contains curcumin, have been shown to have anti-inflammatory properties.
Adequate protein intake is vital for cartilage repair, as it provides the necessary building blocks for tissue regeneration. Patients should ensure they consume sufficient protein from high-quality sources, such as lean meats, fish, eggs, and dairy products.
Proper hydration is also essential for cartilage health, as cartilage is composed of a significant amount of water. Ensuring adequate fluid intake during infrared therapy treatment periods can help maintain cartilage hydration and support its repair.
Various nutritional interventions have been studied for their potential benefits in osteoarthritis management. While some have shown promise, it’s essential to review the current evidence and identify those with the strongest scientific support.
By incorporating these nutritional recommendations into their regimen, patients can take a comprehensive approach to supporting their knee cartilage health alongside infrared therapy.
Combining Infrared Therapy with Other Treatments
Weight management plays a significant role in enhancing the effectiveness of infrared therapy for knee cartilage repair. For patients with knee osteoarthritis, excess weight can exacerbate the condition by increasing the mechanical load on the knee joint.
Weight Management Strategies
The relationship between body weight and knee joint stress is critical. Each pound of weight loss can reduce the load on the knee joint by approximately four pounds, thereby alleviating some of the pressure on the cartilage. This mechanical impact is significant, but it’s not the only way that weight affects knee health.
Adipose tissue, or fat cells, contribute to systemic inflammation, which can negatively impact cartilage health. Therefore, weight management is not just about reducing the mechanical load; it’s also about minimizing the inflammatory effects associated with excess body fat.
A sustainable weight management approach is essential. Gradual, healthy weight loss is more effective in the long term than rapid or extreme dieting. Therapy for knee cartilage repair, including infrared therapy, is more likely to be successful when combined with a healthy weight.
For individuals with knee cartilage damage, low-impact exercises are recommended for weight management. Activities such as swimming, cycling, or using an elliptical machine can help burn calories without putting excessive stress on the knee joint.
Behavioral strategies are also crucial for successful weight management. This includes setting realistic goals, monitoring progress, and maintaining a balanced diet. By combining these strategies with infrared treatment, patients can potentially enhance the benefits of their therapy.
Studies have shown that weight loss can improve outcomes in osteoarthritis treatment. By reducing pain and improving mobility, weight management can complement the effects of infrared therapy, leading to better overall health for individuals with knee osteoarthritis.
The importance of weight management in the context of knee osteoarthritis cannot be overstated. By addressing both the mechanical and inflammatory aspects of excess weight, patients can experience significant improvements in their condition. This comprehensive approach, combining weight management with infrared therapy, offers a promising pathway for managing knee osteoarthritis and improving quality of life.
Monitoring Progress and Adjusting Treatment
To ensure the best results from infrared therapy, we need to systematically monitor our treatment progress. This involves tracking various aspects of our condition to understand how well the therapy is working.
Tracking Pain and Mobility Improvements
One of the primary ways to monitor progress is by tracking pain levels and mobility improvements. Patients undergoing infrared therapy for knee cartilage repair can use various pain assessment tools to monitor their progress. These tools range from simple numeric rating scales to more comprehensive questionnaires specifically designed for knee pain.
Some common pain assessment tools include:
- Numeric Rating Scales (NRS)
- Visual Analog Scales (VAS)
- Knee injury and Osteoarthritis Outcome Score (KOOS)
- Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC)
In addition to pain assessment, objective measures of mobility can be monitored, including range of motion, walking distance, and functional performance tests. It’s essential to maintain consistent assessment timing and conditions to ensure reliable tracking of progress over time.

Distinguishing between temporary fluctuations and meaningful trends in symptoms is crucial for accurate interpretation of progress. Patients should be aware that some days may be better than others, but overall trends are more important than daily variations.
Maintaining a treatment journal can be a practical tool for documenting infrared therapy sessions and corresponding changes in symptoms. By tracking multiple outcome measures, patients can gain a more comprehensive understanding of their treatment response, rather than focusing solely on pain reduction.
For instance, a patient might notice improvements in mobility and reductions in pain, indicating a positive response to the therapy. By systematically tracking these changes, healthcare providers can adjust the treatment protocol as needed to optimize results.
Monitoring Progress and Adjusting Treatment
As patients embark on infrared therapy for knee cartilage repair, knowing what to expect and when is vital. The journey to recovery involves understanding the timeline of effects, from immediate relief to long-term cartilage regeneration.
Timeline for Expected Results
Infrared therapy’s effects on knee cartilage repair manifest at different stages. Immediate effects may include temporary pain relief and improved joint mobility after initial treatments. These early benefits are often encouraging for patients and can be attributed to the therapy’s anti-inflammatory properties.
In the short term, typically after several weeks of consistent treatment, patients may experience more sustained pain reduction and functional improvements. This period is crucial as it indicates the therapy‘s effectiveness in addressing the underlying cartilage damage.
The long-term process of actual cartilage repair and regeneration is more gradual. Studies suggest that noticeable improvements in cartilage health can occur after several months of consistent therapy. However, this timeframe can vary significantly among patients, depending on factors such as the severity of arthritis, overall health, and adherence to the treatment protocol.
Variability in response times is a critical consideration. Factors influencing the rate of progress include the extent of cartilage damage, patient age, and the presence of other health conditions. Understanding these factors helps in setting realistic expectations.
| Timeline | Expected Effects |
|---|---|
| Immediate (After 1-3 sessions) | Temporary pain relief, improved joint mobility |
| Short-term (6-12 weeks) | Sustained pain reduction, functional improvements |
| Long-term (Several months) | Cartilage repair and regeneration |
It’s also important to recognize the concept of treatment plateaus, where progress may seem to slow or stall. This phenomenon can be due to various factors, including the body’s adaptation to the therapy or the natural progression of the underlying condition. Adjusting treatment parameters or combining therapy with other interventions can help overcome these plateaus.
Guidance on reasonable expectations is crucial. For patients with mild arthritis, the response to infrared therapy may be more rapid and pronounced. In contrast, those with more severe degenerative conditions may require longer treatment durations and may benefit from a multi-modal approach.
In conclusion, while the timeline for expected results from infrared therapy for knee cartilage repair can vary, understanding the different stages of effects and the factors influencing them can help patients and healthcare providers monitor progress effectively and make informed decisions about treatment adjustments.
Monitoring Progress and Adjusting Treatment
As we continue our journey with infrared therapy for knee cartilage repair, it’s essential to understand when to adjust treatment parameters to optimize the effectiveness of the therapy.
Modifying Treatment Parameters for Optimal Results
During a course of infrared therapy for knee cartilage repair, it’s crucial to recognize when treatment parameters should be modified to achieve the best possible outcomes for patients. Several signs may indicate that the current protocol is not optimal, including a lack of progress, plateauing of benefits, or adverse reactions.
When adjusting treatment parameters, it’s essential to adopt a systematic approach. This involves changing one variable at a time to identify the most effective adjustments. We must allow sufficient time between modifications to accurately assess their impact on the therapy‘s effectiveness.
Specific parameter adjustments that might be considered include changes to treatment duration, frequency, wavelength, or power density. For instance, if patients are not experiencing the desired effects, we might consider increasing the laser power density or adjusting the wavelength to better target the affected cartilage.
- Assessing the need for adjustments based on patient progress and response to therapy
- Systematically modifying treatment parameters to optimize outcomes
- Considering complementary treatments if infrared therapy alone is not producing sufficient results
- Consulting with healthcare providers about treatment modifications, particularly for patients using at-home devices
In some cases, we may need to consider adding complementary treatments to enhance the effectiveness of infrared therapy for knee cartilage repair, especially for patients with arthritis. This could include physical therapy, nutritional support, or other interventions that promote cartilage health.
By carefully monitoring progress and making informed adjustments to treatment parameters, we can maximize the benefits of infrared laser therapy for patients undergoing knee cartilage repair.
Potential Side Effects and Contraindications
Infrared therapy, while generally safe, can cause some mild side effects in certain patients. As we explore the common mild side effects associated with infrared therapy for knee cartilage repair, it’s crucial to understand that these effects are typically temporary and manageable.
Common Mild Side Effects
Some patients may experience mild side effects during or after infrared therapy. These can include temporary sensations such as mild warmth, tingling, or increased sensitivity in the treatment area. Such effects are usually short-lived and resolve on their own without any need for intervention.
Temporary Sensations During Treatment
During the treatment, patients might feel a gentle warmth or tingling sensation. This is generally considered a normal response to the infrared light and typically subsides shortly after the treatment session.
Short-term Reactions
Following the treatment, some patients may notice temporary redness, mild soreness, or a brief increase in pain. These reactions are usually mild and short-term, resolving quickly without any specific treatment.
| Side Effect | Duration | Management |
|---|---|---|
| Mild warmth or tingling | During treatment | No action required |
| Temporary redness | Few hours post-treatment | Cold compress if necessary |
| Mild soreness | 1-2 days post-treatment | Over-the-counter pain relievers |
To minimize the likelihood of experiencing side effects, proper treatment technique and appropriate parameter selection are crucial. Ensuring that the treatment is administered by a qualified professional can significantly reduce the risk of adverse reactions.
When side effects do occur, managing them effectively is key. For instance, applying a cold compress can help alleviate temporary redness or soreness. In cases where pain is a concern, over-the-counter pain relievers may be recommended, though always under the guidance of a healthcare provider.
Understanding the expected duration of various side effects is essential. Most mild side effects resolve within a few hours to a couple of days. However, if symptoms persist or become severe, it’s crucial to consult with a healthcare provider for further guidance.
Potential Side Effects and Contraindications
Infrared therapy, a promising treatment for knee cartilage repair, comes with specific contraindications that need to be considered to ensure patient safety. As we explore the potential side effects and contraindications of infrared therapy, it’s crucial to understand who should avoid this treatment.
Who Should Avoid Infrared Therapy
Certain individuals should not undergo infrared therapy due to various contraindications. These contraindications can be categorized into absolute and relative contraindications.
Absolute contraindications include conditions where infrared therapy could cause significant harm. These are:
- Active cancer in the treatment area, as laser therapy might stimulate tumor growth.
- Certain photosensitizing medications that could lead to adverse reactions when combined with light therapy.
- Specific skin conditions, such as open wounds or active infections in the treatment area.
Relative contraindications are conditions where infrared therapy may be used with caution and under medical supervision. These include:
- Pregnancy, particularly when treating the abdominal or lower back area.
- Certain autoimmune conditions that might be exacerbated by the treatment.
It’s essential for patients to disclose their complete medical history before beginning infrared therapy to identify potential contraindications. This includes information about implanted medical devices, such as knee replacements or electronic implants, which require special consideration.
Skin pigmentation and sensitivity are also factors that might influence treatment decisions. Patients with darker skin tones or those who are particularly sensitive to light should be monitored closely during therapy.
Healthcare providers should carefully screen patients for contraindications and make appropriate risk-benefit assessments. This involves evaluating the patient’s overall health, the severity of their condition, and the potential benefits of infrared therapy.
| Contraindication Type | Condition | Reason |
|---|---|---|
| Absolute | Active cancer in treatment area | Potential stimulation of tumor growth |
| Absolute | Photosensitizing medications | Risk of adverse reactions |
| Relative | Pregnancy | Potential effects on fetus or pregnancy |
| Relative | Autoimmune conditions | Possible exacerbation of condition |
By understanding these contraindications and taking a cautious approach, healthcare providers can ensure that infraredtherapyis used safely and effectively for knee cartilage repair.
Potential Side Effects and Contraindications
When considering infrared therapy for knee cartilage repair, it’s crucial to understand how it interacts with other treatments patients may be undergoing. Infrared therapy, also known as low-level laser therapy (LLLT) or photobiomodulation (PBM), is increasingly used to promote healing and reduce pain in various conditions, including knee cartilage damage.
Medication Interactions
Infrared therapy may interact with various medications that patients are taking, potentially affecting its efficacy or safety. We need to consider these interactions to provide comprehensive care.
Some medications, known as photosensitizing agents, can increase sensitivity to light. When using infrared therapy, patients on these medications may require adjustments to the treatment parameters to avoid adverse effects. Examples include certain antibiotics, antihistamines, and non-steroidal anti-inflammatory drugs (NSAIDs).
Common pain medications and anti-inflammatory drugs might influence the effectiveness of infrared laser therapy. Some studies suggest that certain NSAIDs may interfere with the biological responses targeted by infrared therapy, such as inflammation reduction and tissue repair.
Topical medications applied to the knee area may also interact with infrared therapy. In some cases, these topical treatments should be removed before infrared therapy sessions to ensure optimal light penetration and effectiveness.
Certain medications can affect the biological responses targeted by infrared therapy. For instance, some drugs may influence cellular metabolism or inflammatory pathways, potentially altering the therapy’s effects.
- To minimize potential interactions, patients should inform their healthcare providers about all medications they are taking, including topical treatments.
- The timing of medication administration in relation to infrared therapy sessions may need to be adjusted based on the specific medications and treatment protocols.
- Healthcare providers should monitor patients for potential interactions and adjust treatment plans accordingly.
By understanding and managing potential interactions between infrared therapy and other medications, healthcare providers can optimize treatment outcomes for patients with knee cartilage damage.
Case Studies: Successful Knee Cartilage Repair
Our examination of case studies reveals that patients with early-stage knee osteoarthritis can significantly benefit from infrared therapy. These cases demonstrate the potential of this treatment to improve symptoms and functional outcomes.
Early-Stage Osteoarthritis Outcomes
Patients with early-stage osteoarthritis typically present with mild to moderate pain and limited functional impairment. Before treatment, these patients often show signs of cartilage degeneration on imaging studies, such as X-rays or MRI.
The infrared therapy protocols used in these cases typically involve treatment sessions 2-3 times a week, with each session lasting between 10-20 minutes. The specific parameters, such as wavelength and power density, are tailored to the individual patient’s needs.
As treatment progresses, patients often report a reduction in pain and improvements in functional ability. These improvements can be attributed to the positive effects of infrared therapy on cartilage health.
| Treatment Parameter | Typical Value | Range |
|---|---|---|
| Wavelength | 810 nm | 780-910 nm |
| Power Density | 50 mW/cm² | 20-100 mW/cm² |
| Treatment Duration | 15 minutes | 10-20 minutes |
Early-stage cases often respond more rapidly and completely to infrared therapy than more advanced disease. Factors contributing to successful outcomes include consistency of treatment and complementary approaches such as physical therapy and nutritional support.
Follow-up data show that the results achieved with infrared therapy can be durable, with many patients maintaining their improvements over time. This suggests that infrared therapy may have a disease-modifying effect in some cases.
Case Studies: Successful Knee Cartilage Repair
Infrared therapy has emerged as a promising treatment for supporting cartilage regeneration in patients with acute knee injuries. This non-invasive approach is being increasingly used as part of comprehensive rehabilitation programs to enhance cartilage repair and improve patient outcomes.
Post-Injury Cartilage Regeneration
The use of infrared therapy in post-injury cartilage regeneration has been explored in various case studies. These studies have focused on patients who have suffered different types of knee trauma, including sports injuries and anterior cruciate ligament tears with associated cartilage damage.
When examining the effectiveness of infrared therapy, it’s crucial to consider how it is integrated into post-injury rehabilitation programs. The timing of initiation and coordination with other treatments play a significant role in determining the outcome.
Infrared therapy is often used in conjunction with other rehabilitation strategies to create a conducive environment for cartilage repair. The progression of cartilage healing is typically documented through imaging studies and functional assessments.
These diagnostic tools provide valuable insights into the effectiveness of infrared therapy in promoting cartilage regeneration. By modulating the inflammatory phase of injury, infrared therapy can potentially create a more favorable environment for cartilage repair.
A comparison of recovery trajectories between cases using infrared therapy and those without this intervention reveals promising results. Patients treated with infrared therapy often show improved cartilage regeneration and faster recovery times.
Key findings from case studies include:
- Enhanced cartilage regeneration in patients treated with infrared therapy following acute knee injuries.
- Improved outcomes in cases involving anterior cruciate ligament tears with associated cartilage damage.
- Faster recovery times and better functional outcomes in patients receiving infrared therapy as part of their rehabilitation program.
By examining these case studies, we can gain a deeper understanding of the role infrared therapy plays in supporting cartilage regeneration and improving outcomes for patients with knee injuries.
Case Studies: Successful Knee Cartilage Repair
Our examination of case studies reveals that multi-modal treatment approaches can significantly enhance knee cartilage repair outcomes. By combining infrared therapy with other treatment modalities, patients have shown improved results in cartilage regeneration and overall knee health.
Enhanced Outcomes with Combination Therapy
We’ve identified several case studies that highlight the benefits of combining infrared therapy with other treatments for knee cartilage repair. These combination approaches have included physical therapy, nutritional interventions, and injections, among others.
The rationale behind these combination protocols is to target multiple aspects of the cartilage repair process. For instance, infrared therapy can stimulate cellular processes, while physical therapy can enhance mechanical stimulation and nutritional interventions can provide essential nutrients for cartilage health.
Synergistic effects have been observed when combining infrared therapy with other treatments. These effects often result in outcomes that are greater than the sum of the individual treatments, leading to more effective cartilage repair.
The sequencing and timing of multiple interventions are critical for optimizing their interaction. In some cases, infrared therapy is administered before or after other treatments to enhance their effectiveness.
- Combination approaches may be particularly beneficial for challenging cases, such as advanced osteoarthritis or complex cartilage defects.
- Cost-benefit considerations are also important when evaluating combination therapies compared to single-modality approaches.
- Patients can make informed decisions about their treatment options by understanding the potential benefits and costs of combination therapies.
By examining these case studies and understanding the principles behind combination therapies, we can better appreciate the potential of infrared therapy to enhance knee cartilage repair when used as part of a comprehensive treatment plan.
Cost Considerations and Insurance Coverage
Infrared therapy, a promising treatment for knee osteoarthritis, comes with various price tags depending on the treatment setting. As patients explore this option for knee cartilage repair, understanding the costs involved is essential.
Average Treatment Costs
The cost of infrared therapy can vary significantly based on several factors, including the treatment environment and the technology used. In clinical settings, the price per session can range widely.
| Treatment Setting | Average Cost per Session | Factors Influencing Cost |
|---|---|---|
| Physical Therapy Practices | $50-$150 | Location, expertise, technology |
| Specialized Pain Clinics | $100-$250 | Technology, staff qualifications |
| Home-use Devices | $200-$1,000 (one-time purchase) | Device quality, brand |
For patients requiring multiple treatment sessions, package pricing and membership models can offer cost savings. It’s also worth comparing the costs of infrared therapy with other common treatments for knee osteoarthritis, such as injections, medications, and surgery.
To manage treatment costs effectively, patients should ask their providers about payment options and potential discounts. Understanding the full scope of costs and benefits is crucial for making informed decisions about infrared therapy for knee cartilage repair.
Cost Considerations and Insurance Coverage
As we explore the financial aspects of infrared therapy for knee cartilage repair, insurance coverage plays a significant role. The extent to which insurance covers this treatment can vary widely depending on several factors.
Insurance Reimbursement Possibilities
Insurance coverage for infrared therapy treatments targeting knee cartilage repair is not uniform across all insurance providers. Different types of insurance plans, including private insurance, Medicare, and Medicaid, may have varying policies regarding coverage for this treatment.
Private insurance plans often have specific guidelines for covering alternative therapies like infrared therapy. Some may cover it as part of a comprehensive physical therapy program, while others may not cover it at all. It’s essential for patients to check their policy details and consult with their insurance provider to determine the extent of their coverage.
For Medicare and Medicaid patients, coverage may be determined by federal and state regulations. Medicare, for instance, may cover certain aspects of physical therapy that include infrared therapy, but the specifics can vary. Medicaid coverage can differ significantly from state to state.
Coding and billing practices also play a crucial role in determining reimbursement for infrared therapy. Healthcare providers must use the correct CPT codes and ensure proper documentation to support the medical necessity of the treatment. Accurate coding can significantly impact the likelihood of successful reimbursement.
When infrared therapy is part of a comprehensive treatment plan, the chances of insurance coverage may increase. This is because it is often considered a supportive therapy rather than a standalone treatment. Working closely with healthcare providers to document the medical necessity of infrared therapy can help maximize the potential for insurance coverage.
For patients facing denied claims, there are strategies to appeal these decisions. Understanding the appeals process and providing additional documentation or justification can sometimes result in overturning the initial denial.
In cases where insurance coverage is not available, patients can explore alternative funding options. Health savings accounts (HSAs), flexible spending arrangements (FSAs), and medical financing programs can provide viable alternatives to help manage the costs of infrared therapy.
As noted by a recent study, “The integration of infrared therapy into treatment plans for knee osteoarthritis has shown promising results, and understanding insurance coverage is crucial for patients seeking this treatment.” This highlights the importance of navigating insurance options effectively.
Cost Considerations and Insurance Coverage
When evaluating infrared therapy for knee cartilage repair, a comprehensive cost-benefit analysis is crucial for making informed decisions. This assessment involves weighing the direct and indirect costs of the treatment against its potential benefits and savings.
Evaluating Long-Term Value
To conduct a thorough cost-benefit analysis, patients must consider several factors. Firstly, they should evaluate the direct costs of infrared therapy, including the cost of the device, maintenance, and any necessary accessories. Additionally, patients should consider the potential savings from reduced medication use, avoided procedures, and delayed or prevented surgery.
Infrared therapy may also yield indirect financial benefits, such as fewer missed workdays, increased productivity, and maintained independence. These factors can significantly impact a patient’s overall quality of life and financial situation.
The non-financial benefits of successful infrared therapy are equally important. Patients may experience improved quality of life, reduced pain, and a greater ability to participate in valued activities. These benefits can have a profound impact on a patient’s overall well-being and should be considered when evaluating the treatment’s value.
When assessing the overall value proposition of infrared therapy, patients must also factor in the time commitment required for treatment. The frequency and duration of treatment sessions can vary, and patients should consider how these demands will fit into their lifestyle.
- Comparing the long-term costs of infrared therapy to other treatment approaches for chronic knee cartilage problems.
- Viewing infrared therapy as an investment in joint health rather than simply an expense.
- Considering the potential long-term benefits of infrared therapy for patients with knee osteoarthritis.
By carefully evaluating these factors, patients can make a more informed decision about whether infrared therapy is a suitable treatment option for their knee cartilage issues. It’s essential to weigh the potential benefits against the costs and consider how this therapy might impact their overall quality of life and financial situation.
For patients with arthritis, particularly those with knee osteoarthritis, infrared therapy offers a promising avenue for managing symptoms and potentially slowing disease progression. By understanding the cost-benefit dynamics of this treatment, patients can better navigate their treatment options and make choices that align with their health goals and financial circumstances.
Future Developments in Infrared Therapy
The future of infrared therapy for knee cartilage repair is being shaped by advancements in technology and our understanding of its biological effects. As we continue to explore the potential of this treatment modality, several emerging technologies and approaches are gaining attention for their potential to enhance treatment outcomes.
Advancements in Light Delivery Systems
One of the key areas of development in infrared therapy is the improvement of light delivery systems. New laser technologies are being designed to offer more precise targeting capabilities, allowing for more effective treatment of specific areas within the knee joint. Additionally, advancements in light penetration depth are enabling more efficient treatment of deeper tissue layers.
These advancements in light delivery systems are crucial for optimizing the effects of infrared therapy on knee cartilage. By improving the precision and depth of light penetration, these new technologies may lead to more significant improvements in cartilage health and function.
Emerging Combination Therapies
Another exciting development in the field of infrared therapy is the emergence of combination devices that integrate laser therapy with other treatment modalities. These may include electrical stimulation or therapeutic ultrasound, among others. The rationale behind these combination therapies is to create a synergistic effect that enhances the overall treatment outcomes for patients with knee cartilage damage.
- Combination of infrared therapy with electrical stimulation to enhance cellular responses
- Integration of therapeutic ultrasound to improve tissue penetration and healing
- Potential for combining infrared therapy with other light-based treatments for enhanced effects
Wearable Infrared Therapy Devices
The development of wearable, continuous low-level infrared therapy devices represents a significant shift towards more convenient and prolonged treatment protocols. These devices allow patients to undergo extended treatment durations while maintaining their normal daily activities, potentially leading to improved outcomes.
Advances in materials science are playing a crucial role in the development of these wearable devices, enabling the creation of more effective, comfortable, and user-friendly infrared therapy systems.
Innovations in Treatment Protocols
Researchers are also exploring new treatment protocols that aim to optimize biological responses through novel timing, pulsing patterns, or wavelength combinations. These innovations are based on a deeper understanding of the effects of photobiomodulation on cellular processes and tissue repair mechanisms.
By tailoring treatment parameters to individual patient needs and responses, clinicians may be able to achieve more consistent and positive outcomes in the future.
As studies continue to elucidate the mechanisms and benefits of infrared therapy, we can expect to see further refinements in treatment approaches and technologies. The future of infrared therapy for knee cartilage repair looks promising, with potential for improved patient outcomes and enhanced quality of life.
Future Developments in Infrared Therapy
The field of infrared therapy is witnessing significant advancements, driven by ongoing clinical trials that are investigating its efficacy for knee cartilage repair and osteoarthritis treatment. These studies are crucial in establishing the therapeutic benefits of infrared therapy, particularly laser therapy, for patients suffering from knee osteoarthritis.
Current Clinical Trials
Several clinical trials are currently underway to assess the effectiveness of infrared laser therapy for knee cartilage repair. These trials are addressing various research questions, from basic efficacy to comparative effectiveness against standard treatments. The trials are also exploring the optimal treatment parameters for different knee cartilage conditions.
Recent trials have shown methodological advances, including more rigorous designs, larger sample sizes, and longer follow-up periods than earlier studies. These advances are helping to establish more reliable evidence for the effectiveness of infrared therapy in treating knee osteoarthritis.
- Novel outcome measures are being used, including advanced imaging techniques to directly assess cartilage changes.
- Multicenter trials are being conducted to establish more generalizable evidence for infrared therapy‘s effectiveness across diverse patient populations.
- Trials are investigating optimal treatment parameters to establish more standardized protocols for specific knee cartilage conditions.
One of the significant aspects of these trials is the use of advanced imaging techniques to assess changes in cartilage health. This approach provides more objective measures of the effects of infrared laser therapy on knee osteoarthritis.
For patients interested in participating in clinical trials of infrared therapy, there are resources available to find appropriate studies. These resources include clinical trial registries and databases that list ongoing and completed trials related to knee osteoarthritis and arthritis treatment.
As these trials continue to produce results, they will provide valuable insights into the potential benefits and limitations of infrared laser therapy for knee cartilage repair. This information will be crucial in shaping future treatment protocols and guidelines for managing knee osteoarthritis.
Future Developments in Infrared Therapy
As infrared therapy continues to evolve, we’re seeing a significant shift towards personalized treatment protocols. This emerging trend is driven by the recognition that individual patient characteristics and specific cartilage conditions can significantly influence treatment outcomes.
Tailoring Treatment to Individual Needs
We’re exploring how genetic factors may influence a patient’s response to infrared therapy. Research suggests that genetic variations can affect the efficacy of laser treatment for knee cartilage repair. By understanding these genetic factors, we may be able to customize treatment protocols to maximize their effectiveness for each patient.
Advanced diagnostic technologies, including specialized imaging and biomarker testing, are also playing a crucial role in personalizing infrared therapy. These technologies help identify the optimal infrared therapy approach for each patient, taking into account the specific characteristics of their knee cartilage damage or arthritis.
- Real-time monitoring of tissue response to adjust treatment parameters
- Artificial intelligence and machine learning to analyze patterns in treatment responses
- Responder phenotyping to identify patients most likely to benefit from specific infrared therapy approaches
The integration of laser therapy with personalized medicine principles is beginning to influence both research and clinical practice. By tailoring treatment protocols to individual patient needs, we can maximize outcomes and improve the overall effectiveness of infrared therapy for knee cartilage repair.
Studies are ongoing to further explore the potential of personalized infrared therapy protocols. These studies aim to provide more insight into the optimal treatment parameters and patient selection criteria for infrared laser therapy.
By embracing this personalized approach, we’re moving towards a future where infrared therapy can be tailored to address the unique needs of each patient, potentially leading to better treatment outcomes and improved quality of life for those suffering from knee cartilage damage or arthritis.
Taking the Next Step with Infrared Therapy
Infrared therapy has emerged as a valuable treatment modality for knee cartilage repair, and we’re here to guide you through the next steps. If you’re considering this treatment for knee pain or arthritis, it’s essential to understand the practical aspects of getting started.
First, finding a qualified provider is crucial. Look for professionals with experience in administering infrared therapy, particularly for knee cartilage repair. When evaluating potential providers, ask about their qualifications, the type of laser or light therapy equipment they use, and their treatment protocols.
A comprehensive assessment before beginning treatment is vital. This initial evaluation will help establish your baseline status and set realistic goals for your treatment. It’s an opportunity to discuss your medical history, the severity of your knee condition, and any previous treatments you’ve undergone.
Developing a personalized treatment plan is the next step. This involves determining the frequency and duration of your infrared therapy sessions, as well as how it will be integrated with other therapies you may be undergoing. Your provider should work with you to tailor a plan that addresses your specific needs and goals.
To prepare for your initial appointment, come informed about your condition and any relevant medical history. Be ready to discuss your symptoms, previous treatments, and what you hope to achieve with infrared therapy. This preparation will help your provider create a more effective treatment plan.
Tracking your progress and maintaining open communication with your healthcare provider are key to successful treatment. Keep a record of your symptoms, treatment sessions, and any changes you notice. This information will be invaluable in adjusting your treatment plan as needed.
Finally, commitment and consistency are crucial. Following through with the recommended treatment protocol will give you the best chance of achieving optimal results. Infrared therapy is not a one-time fix but rather a treatment that requires dedication to a plan.
By taking these steps and working with a qualified provider, you can harness the potential of infrared therapy to support your knee cartilage repair and improve your overall quality of life.
FAQ
What is low-level laser therapy, and how does it work for knee cartilage repair?
Low-level laser therapy, also known as photobiomodulation therapy, is a non-invasive treatment that uses low-intensity laser or light-emitting diodes to stimulate cellular processes, promoting tissue repair and reducing inflammation. We use it to enhance knee cartilage repair by increasing mitochondrial ATP production, reducing oxidative stress, and promoting the synthesis of extracellular matrix.
Is infrared therapy safe for treating knee osteoarthritis?
Yes, infrared therapy is generally considered safe for treating knee osteoarthritis. However, we must consider certain precautions and contraindications, such as avoiding its use over cancerous lesions or in patients with pacemakers. It’s essential to consult with a healthcare professional before starting treatment.
How often should I undergo infrared therapy for knee cartilage repair?
The frequency of infrared therapy sessions can vary depending on the severity of the condition and individual response. Typically, we recommend starting with 2-3 sessions per week and adjusting based on progress and tolerance.
Can I combine infrared therapy with other treatments for knee osteoarthritis?
Yes, we can combine infrared therapy with other treatments, such as physical exercise, nutritional support, and weight management strategies, to enhance its effectiveness. A comprehensive treatment plan can lead to better outcomes and improved overall health.
What are the expected outcomes of infrared therapy for knee cartilage repair?
The expected outcomes of infrared therapy include reduced pain and inflammation, improved mobility, and enhanced cartilage repair. We can monitor progress through regular assessments and adjust the treatment plan as needed.
Are there any potential side effects of infrared therapy for knee cartilage repair?
While generally safe, infrared therapy can cause mild side effects, such as temporary redness or warmth at the treatment site. We should be aware of these potential effects and report any concerns to our healthcare provider.
How long does it take to see results from infrared therapy for knee cartilage repair?
The timeline for expected results can vary depending on individual factors, such as the severity of the condition and treatment frequency. Typically, we can expect to see noticeable improvements within 6-12 weeks of regular treatment.