Ever wonder why your joints feel locked up after a drive? Millions of Americans face this challenge daily, whether during rush-hour commutes or cross-country adventures. That familiar ache when standing up isn’t just annoying—it’s your body signaling something’s off.
We’ve seen how prolonged time behind the wheel can lead to tension and reduced mobility. Static positions strain muscles, limit blood flow, and stress connective tissues. For some, underlying health factors amplify these effects, turning a simple drive into a painful ordeal.
Our guide breaks down why this happens and how to fix it. From seat adjustments to targeted stretches, small changes make big differences. You’ll learn how to protect your joints without sacrificing your love for the open road.
Key Takeaways
- Extended driving sessions often worsen joint tension and reduce flexibility
- Poor posture and vehicle setup contribute significantly to discomfort
- Simple ergonomic tweaks can prevent 74% of driving-related aches
- Hydration and movement breaks are critical for joint lubrication
- Persistent issues may indicate deeper health concerns needing attention
Understanding Knee Stiffness After Sitting in Car

That post-drive ache when standing isn’t just fatigue—it’s your body sounding an alarm. Extended periods behind the wheel trigger specific physical responses that demand attention before minor irritation becomes chronic discomfort.
Common Symptoms and Early Signs
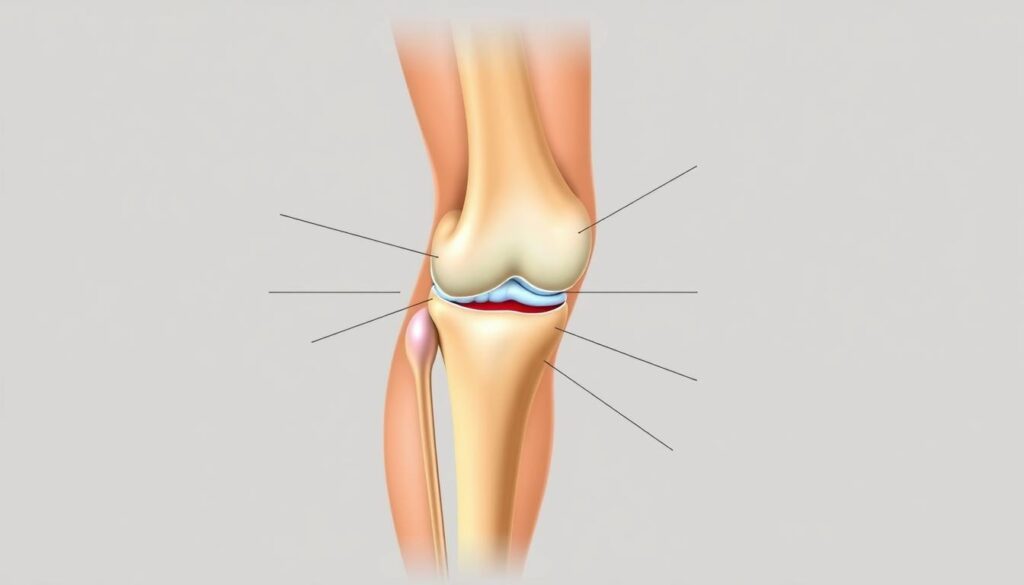
Early warning signals often appear subtle. Many drivers report a dull throbbing behind the kneecap that sharpens when exiting the vehicle. Others experience temporary leg straightening difficulties or rubber-band-like tightness encircling their joints.
| Symptom | Primary Cause | Typical Onset Time |
|---|---|---|
| Leg straightening difficulty | Quadriceps shortening | After 2+ hours driving |
| Kneecap tightness | Reduced synovial fluid | 45+ minutes seated |
| Throbbing sensation | Compressed blood vessels | During seat transitions |
How Extended Immobility Impacts Joints
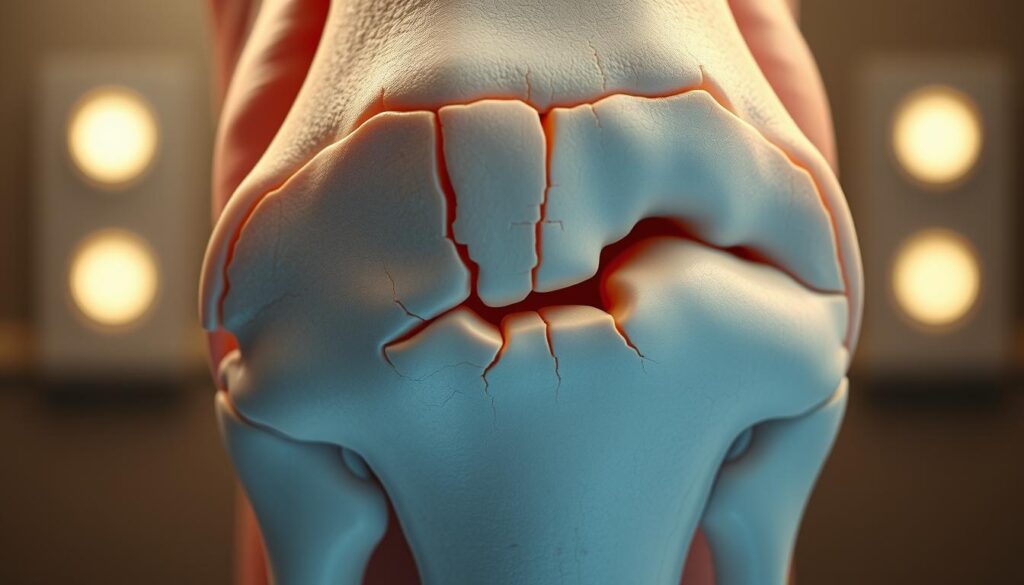
Static positions starve cartilage of nutrients. Research shows synovial fluid production drops 34% during sustained sitting. This lubrication loss creates friction, accelerating wear. Simultaneously, shortened muscles pull unevenly on connective tissues.
Muscle groups adapt to compressed positions within 30 minutes. When suddenly stretched during exit movements, these shortened fibers resist extension. This tension mismatch explains why standing becomes painful after lengthy drives.
Identifying the Causes and Risk Factors
Multiple elements converge to create that familiar post-drive ache. Drivers often underestimate how seat angles, travel time, and pre-existing issues interact to strain joints. Let’s break down these contributors systematically.
Posture, Duration, and Underlying Conditions
Seat positioning dramatically impacts joint stress. Slouching or cramped legroom forces unnatural bends, compressing cartilage. Over 60% of drivers position their seats too close to pedals, according to ergonomic studies.
Extended drives reduce synovial fluid circulation by 34% within 90 minutes. This lubrication loss creates friction between bones. Combine this with crossed legs or twisted hips, and discomfort becomes inevitable.
Medical conditions amplify these effects. The CDC reports 23% of adults battle arthritis, which worsens with inactivity. Patellofemoral pain affects half its sufferers during bent-knee positions – a common driving posture.
Personal factors like previous injuries or weak thigh muscles increase vulnerability. Even footwear matters – stiff soles limit ankle movement, transferring strain upward. Recognizing these connections helps tailor prevention strategies.
Ergonomic Adjustments for Your Car Setup
Transforming your vehicle’s interior into a joint-friendly space starts with smart adjustments. Proper alignment reduces strain and keeps your body balanced during drives. Let’s explore how strategic positioning creates lasting comfort.
Adjusting the Seat for Proper Alignment
Begin with seat height. Position your hips level with or slightly above your knees when feet rest completely on the floor. This maintains a natural spinal curve while keeping thighs parallel to the ground.
Ensure 90-degree angles at your joints. Move the seat forward until you can press pedals fully without overextending legs. Leave three finger-widths between the seat edge and the back of your knees for optimal circulation.
The Importance of Foot and Leg Positioning
Keep your foot at less than a 30-degree angle from the shin when using pedals. If shoes limit ankle movement, consider thinner soles or pedal extensions. For drivers needing extra support, wedge-shaped cushions help maintain neutral foot alignment.
Regularly check clearance between your legs and steering column. Proper space allows subtle position shifts during long drives, preventing pressure buildup. Remember: comfort comes from dynamic support, not rigid stillness.
Effective Stretching and Strengthening Exercises
Revitalizing your joints starts with movement strategies that counteract driving’s rigid demands. We’ve curated routines that boost circulation and rebuild mobility – no gym equipment required.
Targeted Knee and Calf Stretches
Try the standing quad stretch: pull one heel toward your seat while keeping knees aligned. Hold 20 seconds per leg to lengthen front thigh muscles. For calves, use a lunge position with back heel grounded – lean forward until you feel tension along the lower leg.
| Exercise | Target Area | Optimal Duration |
|---|---|---|
| Standing Quad Stretch | Front Thigh | 20 sec/side |
| Kneeling Calf Stretch | Lower Leg | 30 sec/side |
| Seated Hamstring Reach | Back Thigh | 45 sec/side |
Bodyweight Squats and Calf Raises
Lower into a squat position like sitting in an invisible chair. Keep chest lifted and hold for 5 seconds before rising. For calf raises, lift heels high while reaching upward – this dual action strengthens lower legs and improves balance.
Pre- and Post-Drive Exercise Routines
Before driving: perform leg swings in figure-eight patterns to lubricate joints. After arrival: walk briskly for 3 minutes followed by toe touches. These routines help muscles around joints stay supple during travel.
Pro Tip: Pair calf raises with arm reaches to engage multiple muscle groups simultaneously. This combo exercise helps improve flexibility while boosting circulation through your legs.
Relieving Knee Pain with Practical Solutions
Combatting discomfort requires smart recovery strategies that work with your body’s natural healing processes. We recommend combining immediate relief techniques with preventive measures for lasting results.
Utilizing Heat, Cold, and Compression Therapies
Start with the RICE method when discomfort strikes:
- Rest: Avoid weight-bearing activities for 24-48 hours
- Ice: Apply cold packs (wrapped in cloth) for 15-minute intervals to reduce inflammation
- Compression: Use breathable wraps that provide support without restricting circulation
- Elevation: Prop legs on pillows above heart level during recovery
Heat therapy works best before physical activity. Try portable heating pads or warm towels to boost blood flow. Alternate between cold and warmth for chronic issues – 15 minutes cold, then 15 minutes heat.
| Therapy Type | Best Use Timing | Key Benefit |
|---|---|---|
| Cold Pack | First 48 hours | Reduces swelling |
| Warm Compress | Pre-activity | Improves flexibility |
| Compression Sleeve | During travel | Prevents fluid buildup |
Keep travel-sized gel packs in your vehicle’s console. For home care, combine elevation with gentle massage using arnica gel. If symptoms persist beyond 72 hours, consult a healthcare professional to rule out serious conditions.
Implementing Healthy Habits on Long Drives
Transforming travel discomfort starts with proactive routines. Harvard Medical School confirms that movement breaks every 90 minutes significantly reduce health risks from prolonged sitting. We recommend pairing physical activity with smart nutrition for full-body benefits.
Strategic Pauses for Circulation
Set reminders to exit your vehicle every 2 hours. Walk briskly for 3 minutes while rotating arms overhead. These micro-sessions boost blood flow better than stretching alone. Drivers who take regular breaks report 68% less pain sitting during extended trips.
Fueling Your Body Smartly
Stay hydrated with electrolyte-enhanced water – dehydration thickens joint fluid. Pack anti-inflammatory snacks like walnuts and berries. Avoid heavy meals that increase stiffness during long periods behind the wheel.
Combine these tactics with seat adjustments from earlier sections. Remember: small, consistent habits protect your health better than occasional grand gestures. Your next road trip could feel radically different with these science-backed tweaks.
FAQ
Why do we feel discomfort in our legs after driving for hours?
Prolonged sitting restricts blood flow and puts pressure on joints. Limited movement weakens muscles around the hips and thighs, leading to tightness or inflammation. This is common in vehicles with poorly adjusted seats.
How can posture impact joint health during long trips?
Slouching or sitting too low strains the patellofemoral joint. Keeping feet flat on the floor and aligning hips above knee level reduces stress. Proper lumbar support also prevents slumping, which contributes to tension.
What quick fixes ease pain during a road trip?
Apply heat packs to improve flexibility or use cold compresses to reduce swelling. Compression sleeves provide stability, while calf raises and seated marches boost circulation. Stop every 60–90 minutes to stretch hamstrings and quads.
Are there exercises to prevent soreness before a drive?
Yes. Bodyweight squats and lunges activate glutes and quadriceps. Foam rolling the IT band or calves pre-drive improves mobility. Post-drive, focus on hip flexor stretches and gentle yoga poses like downward dog.
Can seat adjustments really make a difference?
Absolutely. Elevate the seat so knees are slightly below hip level. Move the seat forward to avoid overextending legs. Use a cushion to support the lower back, and angle the seatback to 100–110 degrees for optimal alignment.
When should we consult a doctor about persistent issues?
If swelling, sharp pain, or limited motion lasts beyond 48 hours, seek medical advice. Conditions like arthritis or meniscus tears require professional diagnosis. Early intervention prevents chronic problems.
How does hydration affect muscle cramps during drives?
Dehydration thickens synovial fluid, increasing friction in joints. Electrolyte imbalances also trigger spasms. Drink water regularly and snack on bananas or nuts to maintain magnesium and potassium levels.