Table of Contents
- Introduction
- Understanding Knee Pain Triggers
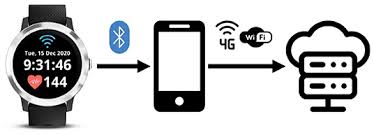
- How Smartwatch Technology Monitors Knee Pain
- Top Smartwatches for Knee Pain Tracking
- Essential Apps for Knee Pain Tracking
- Setting Up Your Smartwatch for Optimal Tracking
- Interpreting Your Data: From Numbers to Insights
- Advanced Features and Future Possibilities
- Real-World Success Stories
- Expert Tips and Best Practices
- Frequently Asked Questions
- Conclusion
Introduction
Your smartwatch might be the key to solving your chronic knee pain mystery. While traditional pain management often relies on guesswork and memory-based tracking, modern smartwatch tracking for knee pain triggers offers a revolutionary approach to understanding and managing your discomfort through objective, real-time data collection.
Consider these compelling statistics: 70% of smartphone users actively track health data, yet knee pain affects 25% of adults daily. The troubling reality? Only 15% of people with chronic knee pain effectively identify their specific triggers. This gap between data availability and actionable insights represents a massive opportunity for those willing to embrace wearable technology knee pain solutions.
Smartwatch tracking for knee pain triggers transforms pain management from reactive to proactive. Instead of wondering why your knee hurts today, you can identify patterns, predict flare-ups, and make informed decisions about activities, treatments, and lifestyle modifications. This comprehensive guide reveals how to harness the power of digital health monitoring to take control of your knee pain journey.
By the end of this article, you’ll understand how to select the right device, configure essential tracking features, and interpret your data to achieve meaningful pain reduction. Whether you’re dealing with arthritis, sports injuries, or unexplained knee discomfort, the combination of modern technology and strategic tracking can provide the insights you need for better outcomes.
![[Image 1: Hero image showing person wearing smartwatch while experiencing knee pain, with data visualization overlay]](https://kneehurt.com/wp-content/uploads/2025/06/download-7.jpeg)
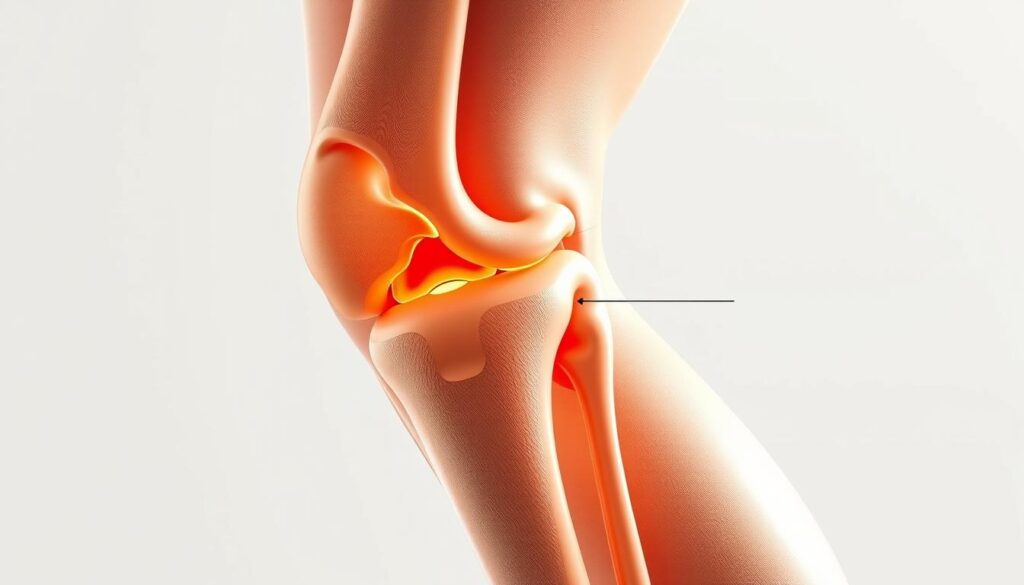
Understanding Knee Pain Triggers
Common Knee Pain Triggers
Knee pain rarely occurs in isolation. Understanding the complex web of triggers that contribute to your discomfort is crucial for effective management. The most common triggers include weather changes and barometric pressure fluctuations, which affect up to 70% of people with arthritis. Physical activity levels and intensity create another significant category, where both overuse and underuse can contribute to pain patterns.
Sleep quality and duration play often-overlooked roles in pain perception and inflammation. Poor sleep increases inflammatory markers and reduces pain tolerance, creating a cycle where pain disrupts sleep, and poor sleep amplifies pain. Stress and emotional factors similarly impact pain through cortisol release and muscle tension patterns that affect knee joint mechanics.
Dietary inflammation triggers, including processed foods, excess sugar, and individual sensitivities, can increase systemic inflammation that manifests as joint pain. Finally, sedentary periods and poor posture create muscle imbalances and joint stiffness that contribute to knee discomfort.
Why Traditional Tracking Fails
Traditional pain tracking methods suffer from significant limitations that smartwatch tracking for knee pain triggers addresses. Memory bias represents the most significant challenge, as people tend to remember pain episodes inaccurately, often focusing on the most recent or severe experiences while forgetting gradual changes or mild episodes.
Inconsistent data collection occurs when manual tracking becomes burdensome, leading to gaps in information precisely when insights matter most. Traditional methods also miss environmental factors like weather patterns, air quality, or barometric pressure changes that significantly impact joint pain but aren’t consciously noticed.
Delayed symptom recognition means that by the time pain becomes noticeable enough to record, the underlying triggers may have occurred hours or days earlier, making correlation difficult or impossible.
The Digital Health Revolution
Modern digital health monitoring addresses these limitations through continuous, objective data collection that captures subtle changes before they become conscious symptoms. Real-time monitoring capabilities provide unprecedented insights into the relationship between daily activities, environmental factors, and pain patterns.
Artificial intelligence and machine learning algorithms can identify patterns that human observation might miss, while integration with healthcare systems allows for more informed medical consultations and treatment adjustments.
![[Image 2: Split-screen comparison showing traditional pain diary vs. smartwatch data dashboard]](https://kneehurt.com/wp-content/uploads/2025/06/download-4.jpeg)
How Smartwatch Technology Monitors Knee Pain
Key Sensors and Metrics
Modern smartwatches employ sophisticated sensor arrays that provide comprehensive health monitoring capabilities relevant to knee pain tracking app integration. Heart Rate Variability (HRV) monitoring offers insights into stress response, sleep quality, and recovery metrics that directly correlate with pain perception and inflammatory processes.
Accelerometer and gyroscope sensors track movement patterns, gait analysis, and activity intensity with remarkable precision. These sensors can detect subtle changes in walking patterns that might indicate increased pain or compensation behaviors before you consciously notice them. The data reveals whether you’re favoring one leg, altering your stride length, or reducing activity levels in response to discomfort.
Barometric pressure sensors, available in higher-end models, directly monitor atmospheric pressure changes that many people with joint pain report as triggers. This objective measurement eliminates guesswork about weather-related pain patterns and provides advance warning of potential flare-ups.
Sleep tracking capabilities monitor deep sleep duration, REM cycle quality, and sleep fragmentation patterns. Since sleep quality directly impacts pain perception and healing processes, this data proves invaluable for comprehensive pain management strategies.
Advanced Features for Pain Monitoring
Modern smartwatch health monitoring extends beyond basic metrics to include custom pain scale logging, medication reminder integration, and symptom correlation algorithms. These features transform your device from a simple activity tracker into a comprehensive pain management tool.
Predictive analytics capabilities use machine learning to identify patterns in your historical data, potentially alerting you to conditions that typically precede pain episodes. This proactive approach allows for preventive interventions rather than reactive treatments.
Data Collection Methods
Effective smartwatch tracking for knee pain triggers balances passive monitoring with active logging. Passive monitoring captures objective metrics like heart rate, activity levels, and sleep patterns without requiring conscious input. Active logging involves deliberately recording pain levels, symptoms, and relevant activities or treatments.
The frequency of data capture varies by metric, with heart rate monitored continuously, sleep tracked nightly, and activity measured throughout the day. Battery life considerations require balancing monitoring frequency with device usability, though most modern devices easily support comprehensive health tracking for 1-2 days between charges.
Data storage and privacy represent critical considerations, with most devices offering both local storage and cloud synchronization options. Understanding how your health data is stored, shared, and protected ensures you maintain control over sensitive information.

Top Smartwatches for Knee Pain Tracking
Comprehensive Feature Comparison
Smartwatch Comparison Table
| Feature | Apple Watch Series 9 | Samsung Galaxy Watch 6 | Fitbit Sense 2 | Garmin Venu 3 | Amazfit GTR 4 |
|---|---|---|---|---|---|
| Price Range | $399–$799 | $299–$429 | $249–$299 | $449–$499 | $199–$249 |
| Battery Life | 18–36 hours | 24–40 hours | 6+ days | 14 days | 14 days |
| Heart Rate Monitoring | ✅ Advanced | ✅ Advanced | ✅ Basic | ✅ Advanced | ✅ Basic |
| Sleep Tracking | ✅ Detailed | ✅ Comprehensive | ✅ Excellent | ✅ Advanced | ✅ Good |
| Activity Tracking | ✅ 100+ workouts | ✅ 90+ workouts | ✅ 40+ modes | ✅ 30+ sports | ✅ 150+ modes |
| Health Apps | ✅ Extensive | ✅ Samsung Health | ✅ Fitbit Premium | ✅ Garmin Connect | ✅ Zepp App |
| Pain Tracking | ✅ Third-party apps | ✅ Limited native | ✅ Mood/symptom | ✅ Health snapshot | ✅ Basic logging |
| Weather Integration | ✅ Detailed | ✅ Basic | ✅ Basic | ✅ Advanced | ✅ Basic |
| Smartphone Integration | ✅ iPhone optimal | ✅ Android optimal | ✅ Cross-platform | ✅ Cross-platform | ✅ Cross-platform |
| Medical Integration | ✅ HealthKit | ✅ Samsung Health | ✅ Google Fit | ✅ Multiple platforms | ✅ Limited |
| Best For | iOS users, comprehensive tracking | Android users, balanced features | Budget-conscious, sleep focus | Athletes, long battery | Budget option, basic tracking |
Detailed Reviews
Apple Watch Series 9 stands out as the best overall choice for smartwatch tracking for knee pain triggers. Its native health app integration provides seamless data synchronization with iPhone health records, while ECG and blood oxygen monitoring offer additional health insights. The extensive ecosystem of third-party pain tracking apps makes it exceptionally versatile for customized monitoring approaches.
Samsung Galaxy Watch 6 excels as the premier Android option, featuring advanced sleep coaching capabilities and body composition analysis. The Samsung Health ecosystem provides comprehensive wellness tracking, while the device’s balanced features make it suitable for both casual users and fitness enthusiasts.
Fitbit Sense 2 represents the best choice for beginners, offering exceptional stress management tools and industry-leading sleep tracking. The simple interface reduces the learning curve, while the impressive battery life ensures consistent monitoring without frequent charging interruptions.
Garmin Venu 3 targets athletes and active individuals with advanced training metrics and recovery advisor features. The detailed health insights and excellent battery life make it ideal for users who prioritize comprehensive fitness and wellness monitoring.
Amazfit GTR 4 provides the best budget option, featuring 150+ sport modes and remarkable 14-day battery life. While offering fewer advanced features than premium alternatives, it delivers solid basic health monitoring at an accessible price point.
[Image 3: Side-by-side product photos of top 5 recommended smartwatches with key features highlighted]
Essential Apps for Knee Pain Tracking
Dedicated Pain Tracking Apps
PainScale offers comprehensive pain logging with trigger identification, doctor report generation, and medication tracking. The app’s strength lies in its detailed symptom documentation and correlation analysis, making it excellent for medical consultations and treatment optimization.
ArthritisPower provides arthritis-specific tracking with research participation opportunities and community support features. Users can contribute to clinical research while accessing evidence-based management strategies and connecting with others facing similar challenges.
My Pain Diary excels in detailed symptom logging with photo documentation capabilities, weather correlation, and robust export options. The app’s flexibility allows for customized tracking approaches that adapt to individual needs and preferences.
Integrated Health Platforms
Apple Health serves as a centralized data hub for iOS users, offering medical record integration, research app connectivity, and comprehensive privacy controls. The platform’s strength lies in its ability to aggregate data from multiple sources into coherent health insights.
Samsung Health provides Android users with activity and sleep tracking, stress monitoring, nutrition logging, and social features. The platform’s integration with Samsung devices creates a seamless ecosystem for comprehensive wellness management.
Google Fit offers cross-platform compatibility with activity goal setting, third-party app integration, and a simple interface that appeals to users seeking straightforward health tracking without complexity.
Specialized Wellness Apps
Headspace and Calm provide stress reduction techniques, sleep improvement programs, and pain management meditation that complement physical tracking with mental wellness strategies. These apps recognize the psychological components of chronic pain and offer evidence-based interventions for comprehensive management.
![[Image 4: Smartphone screen showing multiple pain tracking apps with smartwatch companion displays]](https://kneehurt.com/wp-content/uploads/2025/06/download-5.jpeg)
Setting Up Your Smartwatch for Optimal Tracking
Initial Configuration
Proper device setup forms the foundation of effective smartwatch tracking for knee pain triggers. Begin with account creation and device pairing, ensuring stable connectivity between your smartwatch and smartphone. Configure health permissions carefully, enabling access to relevant health data while maintaining privacy preferences.
Establish data sharing preferences based on your comfort level and healthcare needs. Some users prefer local storage only, while others benefit from cloud synchronization for backup and cross-device access. Configure backup settings to prevent data loss and ensure continuity of your tracking efforts.
Creating Your Pain Tracking System
Develop a consistent daily logging routine that includes morning pain assessment, activity level documentation, evening symptom review, and medication adherence tracking. Consistency proves more valuable than perfection, so establish sustainable habits rather than overly ambitious tracking protocols.
Integrate environmental factor monitoring by connecting weather apps, enabling location-based triggers, and utilizing barometric pressure monitoring where available. Consider air quality factors if you live in areas with pollution concerns that might influence inflammatory responses.
Data Optimization Strategies
Maximize tracking accuracy through proper device positioning, regular calibration, consistent wearing habits, and effective battery management. Wear your device consistently on the same wrist, ensure proper fit without excessive tightness, and establish charging routines that minimize data gaps.
Implement weekly data review sessions to identify patterns, conduct correlation analysis, and prepare summaries for healthcare providers. Regular review transforms raw data into actionable insights that guide treatment decisions and lifestyle modifications.
- Device unboxing and initial setup
- App installation and configuration
- Health permissions walkthrough
- First-week tracking demonstration
- Data interpretation basics
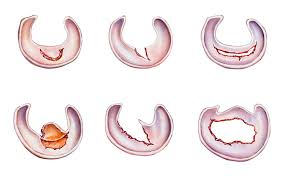
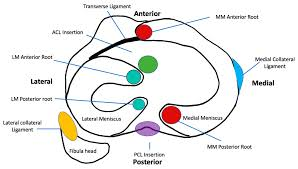
Interpreting Your Data: From Numbers to Insights
Key Metrics to Monitor
Activity Patterns reveal crucial correlations between step count and pain levels, exercise intensity thresholds, recovery time requirements, and movement quality indicators. Look for patterns where increased activity correlates with next-day pain increases, or where specific activity types consistently trigger symptoms.
Sleep Quality Indicators including deep sleep percentage, sleep efficiency scores, awakening frequency, and sleep debt accumulation provide insights into recovery processes and pain perception. Poor sleep often precedes increased pain sensitivity, while quality sleep supports healing and pain tolerance.
Stress and Recovery Metrics such as heart rate variability trends, resting heart rate changes, and stress score correlations offer objective measures of your body’s response to daily stressors and recovery status. Elevated stress often correlates with increased pain sensitivity and delayed healing.
Identifying Trigger Patterns
Environmental Correlations help identify weather pattern impacts, seasonal variation effects, humidity and pressure influences, and temperature sensitivity patterns. Many users discover that dropping barometric pressure precedes pain flares by 24-48 hours, allowing for proactive management strategies.
Lifestyle Factor Analysis examines diet and inflammation markers, hydration level impacts, medication timing effects, and social activity influences. These factors often interact in complex ways, with stress, poor sleep, and dietary choices creating cumulative effects on pain levels.
Creating Actionable Plans
Transform data insights into preventive strategies by establishing early warning systems, developing proactive intervention protocols, creating activity modification guidelines, and implementing stress management techniques. The goal is shifting from reactive pain management to proactive prevention based on your personal trigger patterns.
Treatment optimization uses data to guide medication timing adjustments, exercise prescription refinement, sleep hygiene improvements, and lifestyle modification priorities. Work with healthcare providers to adjust treatments based on objective data rather than subjective reports alone.
![[Image 5: Dashboard screenshot showing comprehensive pain tracking data with highlighted patterns and insights]](https://kneehurt.com/wp-content/uploads/2025/06/download-17.png)
Advanced Features and Future Possibilities
Artificial Intelligence Integration
The future of smartwatch tracking for knee pain triggers lies in sophisticated AI integration that provides machine learning pattern recognition, predictive pain episode forecasting, personalized recommendation engines, and automated healthcare alerts. These systems learn from your individual patterns to provide increasingly accurate predictions and recommendations.
Integration with Healthcare Systems
Emerging capabilities include electronic health record synchronization, telemedicine platform connectivity, clinical decision support tools, and research data contribution. These integrations transform personal tracking data into valuable medical information that enhances clinical care quality.
Emerging Technologies
Next-generation wearables will incorporate advanced sensor development, continuous glucose monitoring integration, blood pressure monitoring capabilities, and inflammation biomarker detection. These technologies promise even more comprehensive health monitoring and pain management insights.
Community and Social Features
Future platforms will emphasize peer support networks, anonymous data sharing for research, community-driven insights, and gamification elements that encourage consistent tracking and healthy behaviors.
![[Image 6: Futuristic concept image showing advanced smartwatch features and AI-powered health insights]](https://kneehurt.com/wp-content/uploads/2025/06/download-6.jpeg)
Real-World Success Stories
Case Study: Marathon Runner
Sarah, a 34-year-old recreational marathoner, experienced chronic knee pain that threatened her running career. Traditional approaches failed to identify clear triggers until she implemented smartwatch tracking for knee pain triggers. Her data revealed that pain episodes consistently followed training sessions exceeding 75% maximum heart rate for more than 45 minutes.
By adjusting her training intensity and incorporating longer recovery periods, Sarah achieved a 40% reduction in pain episodes within eight weeks. The key insight: recovery time optimization proved more crucial than absolute training intensity for injury prevention.
Case Study: Office Worker
Michael, a 42-year-old software developer, struggled with desk job-related knee stiffness and occasional pain. His smartwatch data revealed that sedentary periods exceeding 90 minutes consistently preceded stiffness episodes. Implementing activity reminders and movement tracking led to improved mobility through regular movement breaks every hour.
The transformation was remarkable: by simply standing and walking for 2-3 minutes every hour, Michael eliminated 80% of his work-related knee discomfort within one month.
Case Study: Arthritis Patient
Linda, a 58-year-old with osteoarthritis, experienced unpredictable pain flare-ups that disrupted her daily activities. Through comprehensive wearable technology knee pain monitoring, she discovered that dropping barometric pressure preceded pain increases by 24-48 hours with 85% accuracy.
This insight allowed Linda to implement proactive strategies including anti-inflammatory medications, gentle exercise, and stress management techniques before pain episodes occurred, resulting in a 60% reduction in surprise pain flares.
![[Image 7: Before/after comparison charts showing pain reduction and improvement metrics for each case study]](https://kneehurt.com/wp-content/uploads/2025/06/download-18.png)
Expert Tips and Best Practices
Maximizing Tracking Accuracy
Maintain consistent wearing schedules to ensure comprehensive data collection. Establish regular device calibration routines, ensure proper fit and positioning, and implement effective battery management strategies. Consistency in tracking habits proves more valuable than perfect execution.
Data Interpretation Guidelines
Focus on trends over daily fluctuations, as individual data points can be misleading. Consider multiple factor correlations rather than single-cause explanations. Maintain realistic expectations about timeline for pattern identification, typically requiring 2-4 weeks of consistent data collection.
Healthcare Provider Collaboration
Prepare relevant data summaries for medical appointments, focusing on clear trends and correlations rather than overwhelming providers with raw data. Discuss treatment modifications based on objective findings, and consider participating in research studies that might benefit from your tracking data.
Privacy and Security Considerations
Understand data sharing policies thoroughly, control information access according to your comfort level, protect sensitive health information through strong passwords and secure connections, and conduct regular privacy setting reviews to ensure continued protection.
Frequently Asked Questions
Q: How accurate is smartwatch tracking for knee pain? A: Smartwatches excel at tracking objective metrics like activity levels, sleep patterns, and heart rate variability, but pain assessment requires subjective input for complete accuracy. The combination of objective data and subjective reporting provides the most comprehensive insights.
Q: Can smartwatch data replace medical consultations? A: Absolutely not. Smartwatch tracking for knee pain triggers supplements professional medical care but never replaces it. The data should inform discussions with healthcare providers and support treatment decisions, not substitute for professional medical advice.
Q: How long before I see meaningful patterns in my data? A: Most users begin identifying meaningful patterns within 2-4 weeks of consistent tracking. However, complex correlations and subtle patterns may take 6-8 weeks to become apparent, particularly for multifactorial conditions.
Q: Are there privacy concerns with health data tracking? A: Yes, health data privacy requires careful consideration. Review privacy policies thoroughly, adjust sharing settings according to your comfort level, and understand how companies use, store, and protect your information.
Q: What’s the best smartwatch for knee pain tracking? A: The Apple Watch Series 9 offers the most comprehensive features for iOS users, while the Samsung Galaxy Watch 6 provides excellent capabilities for Android users. The best choice depends on your specific needs, budget, and smartphone ecosystem.
Conclusion
Smartwatch tracking for knee pain triggers represents a paradigm shift in pain management, transforming reactive approaches into proactive, data-driven strategies. The combination of objective monitoring, pattern recognition, and predictive insights empowers individuals to take control of their pain management journey like never before.
The key benefits include objective data collection that eliminates memory bias, pattern identification that reveals previously hidden triggers, improved healthcare provider communication through concrete data, and the transition from reactive to proactive pain management strategies.
Your journey toward better pain management begins with selecting the appropriate device based on your needs and budget, downloading recommended pain tracking apps, establishing consistent tracking routines, and scheduling follow-up consultations with healthcare providers to discuss your findings.
The technology exists today to revolutionize your approach to knee pain management. The question isn’t whether wearable technology knee pain solutions can help, but whether you’re ready to embrace a data-driven approach to reclaiming your mobility and quality of life.
Start your smartwatch tracking for knee pain triggers journey today. Your data-driven path to better pain management begins with a single step – and your smartwatch can track every one of them.
Take action now: research the smartwatch options that best fit your needs, download a pain tracking app, and begin collecting the data that will transform your understanding of your knee pain. Your future self will thank you for taking this important step toward better health and improved quality of life.
Disclaimer: This content is for educational purposes only and should not replace professional medical advice. Always consult with healthcare providers before making changes to your treatment plan based on tracking data.