Welcome to our comprehensive guide on knee osteoarthritis, a degenerative joint disease that affects millions of people. In this first section, we will explore the onset timing of knee osteoarthritis and provide valuable insights into when it starts.
Knee osteoarthritis can be divided into two types: primary and secondary. Primary osteoarthritis occurs without any apparent underlying reason, while secondary osteoarthritis is the result of abnormal force or cartilage abnormalities in the joint.
Most commonly seen in the elderly, knee osteoarthritis is characterized by symptoms such as knee pain, stiffness, swelling, and reduced mobility. To effectively manage these symptoms and provide appropriate treatment, understanding the onset timing of knee osteoarthritis is crucial.
In the next sections, we will delve deeper into the early signs of knee osteoarthritis, the timeline of knee joint degeneration, and how to identify the disease in its early stages. We will also explore the causes, risk factors, and prevalence of knee osteoarthritis, as well as the pathophysiology behind its development.
Join us on this journey as we uncover valuable information about knee osteoarthritis and empower you to take control of your joint health.
Early Signs of Knee Osteoarthritis
In the early stages of knee osteoarthritis, individuals may not experience noticeable symptoms. However, there are some early signs that may indicate the onset of the disease.
- Mild discomfort: Some individuals may experience mild discomfort in the knee joint, which can be easily overlooked or attributed to other factors.
- Stiffness in the knee joint: Stiffness, especially after a period of rest or inactivity, can be an early sign of knee osteoarthritis.
- Pain after prolonged sitting or resting: If you feel pain or stiffness in the knee after sitting or resting for an extended period, it may be an early symptom of knee osteoarthritis.
- Pain that worsens with activity: As the disease progresses, pain in the knee joint may worsen during activities such as walking, climbing stairs, or engaging in sports.
- Pain that gradually worsens over time: Knee pain that gradually becomes more frequent and intense over time is a common early sign of knee osteoarthritis.
It is important to pay attention to these early signs and seek medical attention for proper diagnosis and management. Early intervention can help slow down the progression of knee osteoarthritis and improve long-term outcomes.
Timeline of Knee Joint Degeneration
Knee joint degeneration in osteoarthritis is a progressive process that unfolds over time. Although the timeline of degeneration may vary for each individual, there is a general pattern that can serve as a guide to understand the progression of the disease. The stages of knee joint degeneration and their corresponding symptoms are as follows:
- Early Stages: During this phase, the cartilage in the knee joint may already be damaged, but symptoms may not be noticeable. It is during this stage that the disease often goes undiagnosed, making early intervention challenging.
- Progression: As the disease advances, symptoms such as knee pain, stiffness, and swelling become more frequent and severe. The joint space begins to narrow, cartilage continues to break down, and bone spurs may develop.
- Advanced Stages: In the later stages of knee joint degeneration, there is significant cartilage loss, leading to bone-on-bone friction within the joint. This stage is often characterized by intense pain and discomfort, limiting mobility and impacting the quality of life for individuals with knee osteoarthritis.
The timeline of knee joint degeneration provides valuable insights into the progression of knee osteoarthritis and helps healthcare professionals develop appropriate management strategies for patients. Understanding the different stages allows for early intervention, potentially slowing down the degenerative process and providing relief for those affected by knee osteoarthritis.

Quote:
“By understanding the timeline of knee joint degeneration in osteoarthritis, we can offer tailored treatment plans that address the specific needs of each patient at different stages of the disease progression.”
– Dr. Emily Smith, Orthopedic Surgeon
Identifying Early Knee Osteoarthritis
Identifying early knee osteoarthritis can be challenging as symptoms may be subtle or non-existent in the early stages. However, there are certain risk factors that can increase the likelihood of developing the disease. These include:
- Age: Knee osteoarthritis is more common in older adults.
- Genetics: A family history of knee osteoarthritis can increase the risk.
- Gender: Females are more prone to knee osteoarthritis.
- Obesity: Excess weight places additional stress on the knee joint.
- Previous knee injuries: Injuries like ligament tears or fractures can contribute to the development of osteoarthritis.
To identify early signs of knee osteoarthritis, it is crucial to schedule regular check-ups with a healthcare provider. They can assess joint health and perform diagnostic tests, such as imaging studies and physical examinations. Monitoring for symptoms like knee pain, stiffness, swelling, clicking sounds, or limited mobility is essential. This proactive approach allows for early intervention and treatment, improving the outcomes for individuals at risk of knee osteoarthritis.
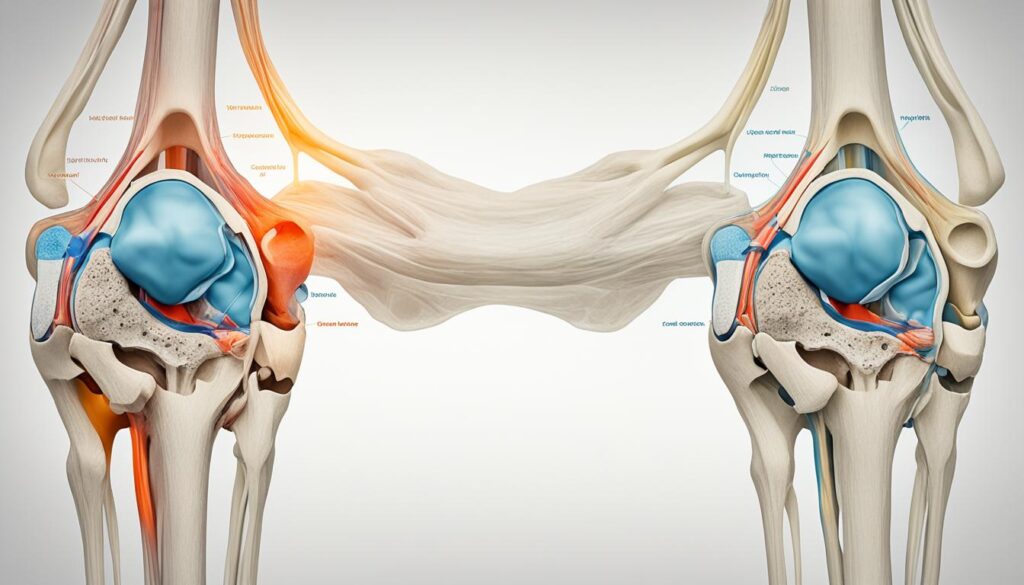
Table: Risk factors for knee osteoarthritis
| Risk Factors | Description |
|---|---|
| Age | Knee osteoarthritis is more common in older adults. |
| Genetics | A family history of knee osteoarthritis increases the risk. |
| Gender | Females are more prone to knee osteoarthritis. |
| Obesity | Excess weight places additional stress on the knee joint. |
| Previous knee injuries | Injuries like ligament tears or fractures can contribute to the development of osteoarthritis. |
Causes and Risk Factors of Knee Osteoarthritis
Knee osteoarthritis can develop due to various causes and risk factors. Understanding these factors can help us identify individuals who may be more susceptible to this condition and take appropriate preventive measures.
Age and Wear and Tear
One of the primary risk factors for knee osteoarthritis is age. As we grow older, the natural wear and tear on our joints can lead to the degradation of knee cartilage. Over time, this can result in osteoarthritis affecting the knees.
Genetics
Our genetic makeup can also play a role in the development of knee osteoarthritis. Certain genetic traits may make individuals more prone to this condition.
Obesity and Excessive Stress
Obesity is another significant risk factor for knee osteoarthritis. The excess weight places additional stress on the knee joint, accelerating the wear and tear process and increasing the likelihood of cartilage deterioration.
Previous Knee Injuries
Individuals who have experienced previous knee injuries, such as ligament tears or fractures, have an increased risk of developing osteoarthritis in the affected knee. These injuries can lead to lasting damage that contributes to the onset of the condition.
Abnormal Joint Structure
Abnormalities in joint structure, such as malalignment or misshapen bones, can also contribute to the development of knee osteoarthritis. These structural irregularities can create uneven pressure distribution within the joint, leading to cartilage wear and tear over time.
To summarize, the causes and risk factors of knee osteoarthritis include age, genetics, obesity, previous knee injuries, and abnormalities in joint structure. Understanding these factors can help us identify individuals at higher risk and implement strategies to prevent or manage the condition effectively.
| Risk Factors | Impact on Knee Osteoarthritis |
|---|---|
| Age | Increases the risk due to wear and tear accumulation |
| Genetics | May make individuals more susceptible |
| Obesity | Excessive weight places added stress on the knee joint |
| Previous Knee Injuries | Increases the likelihood of osteoarthritis development |
| Abnormal Joint Structure | Uneven pressure distribution can lead to cartilage wear |
Prevalence of Knee Osteoarthritis
Knee osteoarthritis is a prevalent condition, particularly among the elderly population. The prevalence of knee osteoarthritis increases with age, and it is estimated that roughly 13% of women and 10% of men aged 60 and older have symptomatic knee osteoarthritis. Among those over the age of 70, the prevalence can be as high as 40%. It’s important to note that not everyone with radiographic evidence of knee osteoarthritis experiences symptoms.
The incidence of symptomatic knee osteoarthritis is approximately 240 cases per 100,000 people per year. As the population continues to age, the number of individuals affected by knee osteoarthritis is expected to rise. Early detection, diagnosis, and management are crucial for improving the quality of life for those with knee osteoarthritis.
Regular check-ups with a healthcare provider and maintaining a healthy lifestyle can help minimize the impact of knee osteoarthritis and prevent complications. By understanding the prevalence of knee osteoarthritis and its impact on individuals, we can work towards developing effective strategies for prevention, early intervention, and comprehensive management of this common condition.
Our commitment is to provide accurate information and guidance to help you navigate the challenges of living with knee osteoarthritis and ensure that you receive the best possible care.
Pathophysiology of Knee Osteoarthritis
The pathophysiology of knee osteoarthritis involves the progressive degradation of articular cartilage in the knee joint. While the exact mechanisms underlying the development of osteoarthritis are not fully understood, research suggests that an imbalance between cartilage degradation and repair processes contributes to its onset and progression.
Over time, knee osteoarthritis results in the loss of collagen, a key structural protein, and proteoglycans, which are essential for maintaining cartilage elasticity. This loss leads to a decrease in the overall integrity and functionality of the cartilage, making it more susceptible to damage. As a result, the knee joint may experience increased friction and joint space narrowing, further exacerbating the degenerative process.
In addition to cartilage degeneration, bone spurs can develop as a response to the changes in the joint. These spurs, also known as osteophytes, can further contribute to pain and stiffness by impinging on surrounding structures. The presence of inflammation within the joint, characterized by increased levels of inflammatory mediators, such as cytokines and chemokines, may also play a role in the progression of knee osteoarthritis.
Overall, the pathophysiology of knee osteoarthritis involves a complex interplay of factors that contribute to cartilage degradation and joint degeneration. Further research is needed to fully understand the molecular and cellular processes involved, which could ultimately lead to the development of more targeted and effective treatment strategies.
Next, let’s take a closer look at some of the risk factors that contribute to the development of knee osteoarthritis and how it can be identified in its early stages.
Conclusion
Knee osteoarthritis is a progressive disease that can significantly impact your quality of life. However, by understanding the onset timing and progression of knee osteoarthritis, you can take proactive steps to effectively manage your symptoms.
If you experience knee pain or other symptoms, it is important to seek medical attention for early intervention. This can help slow down the progression of the disease and prevent further damage to your knee joint.
When it comes to managing knee osteoarthritis symptoms, conservative treatment options such as physical therapy, pain management, and lifestyle modifications are often the first line of defense. These approaches focus on improving joint function, reducing pain, and increasing mobility.
In some cases, surgical interventions may be necessary to alleviate pain and improve joint function. Your healthcare provider will be able to guide you on the most appropriate treatment options for your specific situation.
By taking a comprehensive approach to knee osteoarthritis management, you can maintain an active and fulfilling lifestyle, despite the challenges posed by the condition. Remember to prioritize self-care, follow your healthcare provider’s recommendations, and stay proactive in managing your knee osteoarthritis symptoms.
FAQ
When does knee osteoarthritis begin?
Knee osteoarthritis typically begins as a result of wear and tear and progressive loss of articular cartilage. It can start at any age but is most common in older adults.
What are the early signs of knee osteoarthritis?
Early signs of knee osteoarthritis may include mild discomfort, stiffness in the knee joint, pain after prolonged sitting or resting, pain that worsens with activity, and pain that gradually worsens over time.
What is the timeline of knee joint degeneration in osteoarthritis?
The timeline of knee joint degeneration varies for each individual, but generally follows a pattern. In the early stages, cartilage damage may be present but symptoms may not be noticeable. As the disease progresses, symptoms such as knee pain, stiffness, and swelling become more frequent and severe.
How can I identify early knee osteoarthritis?
Identifying early knee osteoarthritis can be challenging as symptoms may be subtle or non-existent. However, certain risk factors such as age, genetics, obesity, previous knee injuries, and abnormalities in joint structure can increase the likelihood of developing the disease.
What causes knee osteoarthritis?
Knee osteoarthritis can be caused by a combination of factors, including age, genetics, obesity, previous knee injuries, and abnormalities in joint structure. The risk of developing knee osteoarthritis increases with age and obesity can contribute to the development of the disease by placing excessive stress on the knee joint.
What is the prevalence of knee osteoarthritis?
Knee osteoarthritis is a common condition, particularly among the elderly population. It is estimated that roughly 13% of women and 10% of men aged 60 and older have symptomatic knee osteoarthritis.
What is the pathophysiology of knee osteoarthritis?
The pathophysiology of knee osteoarthritis involves the progressive degradation of articular cartilage in the knee joint. The exact mechanisms underlying the development of osteoarthritis are not fully understood, but an imbalance between cartilage degradation and repair processes is believed to play a role.
How can I manage knee osteoarthritis symptoms?
Managing knee osteoarthritis symptoms typically involves a comprehensive approach. Conservative treatment options, such as physical therapy, pain management, and lifestyle modifications, are usually recommended as initial approaches. In some cases, surgical interventions may be necessary to alleviate pain and improve joint function.
Leave a Reply