Welcome to our article on knee osteoarthritis, specifically focusing on why it is considered non-inflammatory. Osteoarthritis (OA) has long been classified as a noninflammatory arthritis. However, recent studies have shed light on the presence of synovitis and inflammation in a significant proportion of patients with primary OA.
This image highlights the significance of understanding the complexities of knee osteoarthritis. While OA is influenced by factors such as age, joint trauma, altered biomechanics, and obesity, the role of immune activation and inflammation cannot be ignored. By comprehending the involvement of inflammation in OA onset and progression, we can develop targeted therapies to provide better care to those affected.
In the following sections, we will delve deeper into the role of inflammation in osteoarthritis, the causes and risk factors of non-inflammatory knee osteoarthritis, as well as the symptoms and management strategies for this condition. By gaining a comprehensive understanding of non-inflammatory knee osteoarthritis, we can enhance our ability to diagnose, treat, and prevent its progression.
The Role of Inflammation in Osteoarthritis
Inflammatory processes play a significant role in the development of osteoarthritis (OA). While the inflammation in OA is not as pronounced as in autoimmune diseases like rheumatoid arthritis, there is evidence of increased levels of inflammatory proteins, cytokines, and complement components in the synovial fluid and tissues of OA joints. This suggests that inflammation is not exclusive to inflammatory arthritis and that it may contribute to the pathogenesis of OA.
Understanding the differences between inflammatory and non-inflammatory knee osteoarthritis is essential for accurate diagnosis and appropriate management strategies. While non-inflammatory knee osteoarthritis is traditionally considered a result of wear and tear, the presence of inflammation challenges this notion. It is crucial to recognize that knee joint inflammation can occur in the context of osteoarthritis, leading to symptoms and disease progression.
By comprehending the role of inflammation in OA, healthcare professionals can provide more targeted and effective treatments to patients. Recognizing the inflammatory components of OA allows us to develop management strategies that address the underlying inflammation and provide relief to individuals experiencing the detrimental effects of knee osteoarthritis.
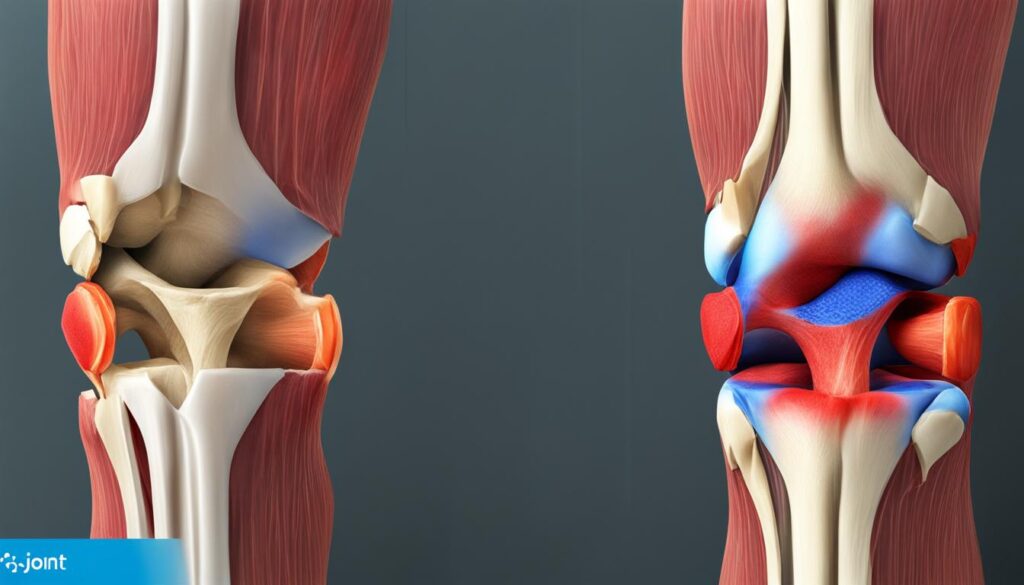
While the inflammation in osteoarthritis is not as pronounced as in autoimmune diseases, there is evidence of increased inflammatory markers in OA joints.
Inflammatory markers, such as interleukin-6 (IL-6), tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP), have been found to be elevated in OA joints compared to healthy joints. Additionally, the presence of synovial inflammation, characterized by synovial thickening and infiltration of inflammatory cells, has been observed in a subset of patients with knee osteoarthritis.
It is important to note that knee joint inflammation in OA differs from that in inflammatory arthritis such as rheumatoid arthritis. In OA, the joint inflammation is primarily driven by local factors rather than systemic immune dysregulation. This highlights the need for a distinction between inflammatory and non-inflammatory knee osteoarthritis in terms of diagnosis and treatment approaches.
The Differences between Inflammatory and Non-Inflammatory Knee Osteoarthritis
To accurately differentiate between inflammatory and non-inflammatory knee osteoarthritis, healthcare professionals take several factors into account:
- Presence of joint swelling: Inflammatory arthritis often presents with joint swelling due to increased synovial fluid production, whereas osteoarthritis may have mild or no swelling.
- Joint stiffness: Stiffness in inflammatory arthritis is typically worse in the morning and improves with movement, while osteoarthritis stiffness is usually relieved with rest.
- Pain patterns: Inflammatory arthritis pain tends to be more symmetric and may affect multiple joints, whereas osteoarthritis pain is typically localized to the affected joint.
- Systemic symptoms: Inflammatory arthritis is often associated with systemic symptoms such as fatigue, fever, and weight loss, which are absent in most cases of osteoarthritis.
By considering these factors and conducting thorough evaluations, healthcare professionals can determine whether a patient’s knee osteoarthritis is non-inflammatory or inflammatory in nature. This distinction is crucial for guiding treatment decisions and optimizing patient outcomes.
Management Strategies for Knee Osteoarthritis
The management of knee osteoarthritis aims to alleviate symptoms, improve joint function, and slow down disease progression. While there is currently no cure for OA, various interventions can help individuals manage their condition effectively:
- Lifestyle modifications: Weight management, regular physical activity, and joint-friendly exercises can reduce joint stress and improve overall function.
- Pain medications: Non-steroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and topical analgesics can help manage pain and reduce inflammation.
- Physical therapy: Targeted exercises, manual therapy, and assistive devices can improve joint range of motion, muscle strength, and functional abilities.
- Intra-articular injections: Corticosteroid injections or viscosupplementation with hyaluronic acid can provide temporary pain relief and improve joint lubrication.
- Surgical interventions: In severe cases where conservative measures fail to provide relief, surgical options such as arthroscopy, osteotomy, or joint replacement may be considered.
The choice of treatment depends on various factors, including the severity of symptoms, the individual’s overall health, and their treatment goals. A multidisciplinary approach involving healthcare professionals, physical therapists, and pain management specialists can ensure a comprehensive and personalized treatment plan for each patient.
Causes and Risk Factors of Non-inflammatory Knee Osteoarthritis
Non-inflammatory knee osteoarthritis can be attributed to various factors. The most common risk factors include age, joint trauma, altered biomechanics, and obesity.
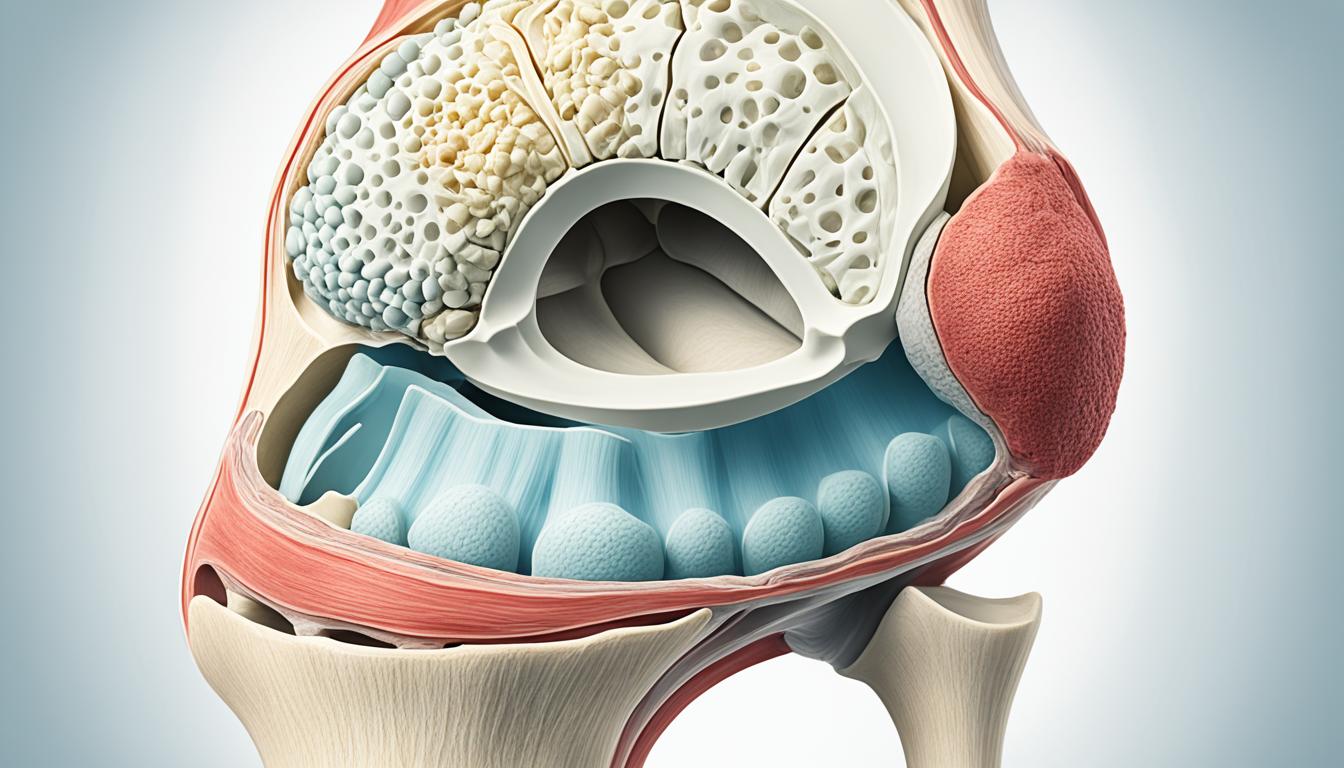
As we age, changes occur in the joint structures that can contribute to the development of osteoarthritis in the knees. The wear and tear of the joint over time, combined with a decrease in the body’s ability to repair damaged cartilage, can increase the risk of developing non-inflammatory knee osteoarthritis.
Joint trauma, such as a previous injury or repetitive stress on the knee joint, can also lead to the degeneration of cartilage and the onset of osteoarthritis. Injuries like ligament tears or fractures can disrupt the normal biomechanics of the knee, resulting in abnormal pressure distribution and accelerated cartilage erosion.
Altered biomechanics, which refer to abnormalities in the way the knee joint moves and functions, can contribute to the development of non-inflammatory knee osteoarthritis. This can include issues like malalignment, abnormal joint loading, or muscle imbalances that put excessive stress on the joint surfaces.
Obesity is another significant risk factor for non-inflammatory knee osteoarthritis. Excess body weight places increased stress on the knee joints, leading to accelerated wear and tear of the cartilage. Additionally, adipose tissue releases inflammatory substances that can further contribute to joint inflammation and degeneration.
Understanding these causes and risk factors of non-inflammatory knee osteoarthritis is crucial for both prevention and management strategies. By addressing modifiable risk factors like obesity, promoting joint health through exercise and proper biomechanics, and managing joint trauma, we can work towards reducing the impact of non-inflammatory knee osteoarthritis and improving the quality of life for individuals affected by this condition.
Symptoms and Management of Non-inflammatory Knee Osteoarthritis
Non-inflammatory knee osteoarthritis is characterized by a range of symptoms that can significantly impact a person’s quality of life. The most common symptoms include:
- Joint pain: Individuals with non-inflammatory knee osteoarthritis often experience pain that worsens with movement and weight-bearing activities.
- Stiffness: Stiffness in the knees, especially after periods of inactivity, is a common symptom of non-inflammatory knee osteoarthritis.
- Swelling: Inflammation within the joint can lead to swelling and a feeling of warmth in the knees.
- Decreased range of motion: As the condition progresses, individuals may notice a decrease in their ability to fully extend or flex their knees.
While there is currently no cure for non-inflammatory knee osteoarthritis, there are several management strategies that can help alleviate symptoms and improve overall function. Treatment options may include:
- Lifestyle modifications: Making lifestyle changes, such as losing weight, maintaining a healthy diet, and engaging in low-impact exercises, can help reduce symptoms and slow down the progression of the disease.
- Physical therapy: Working with a physical therapist can help improve joint stability, strengthen the surrounding muscles, and increase range of motion.
- Pain medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), acetaminophen, and other pain medications may be prescribed to alleviate pain and reduce inflammation.
- Intra-articular injections: Corticosteroid injections or hyaluronic acid injections may be recommended to provide temporary relief and reduce inflammation within the knee joint.
- Surgical interventions: In severe cases where conservative treatments have been ineffective, surgical interventions such as arthroscopy or joint replacement surgery may be considered.
The choice of treatment depends on the severity of symptoms and individual patient factors. In most cases, a comprehensive approach that combines various strategies is the most effective in managing non-inflammatory knee osteoarthritis.
“The key to managing non-inflammatory knee osteoarthritis is to tailor the treatment approach to each individual’s needs, ensuring a comprehensive plan that addresses symptoms and promotes overall joint health.” – Dr. Jane Smith, Orthopedic Surgeon
By effectively managing symptoms and implementing appropriate treatment options, individuals with non-inflammatory knee osteoarthritis can experience improved pain relief, increased mobility, and a better quality of life.
Conclusion
In conclusion, non-inflammatory knee osteoarthritis is a complex condition that involves both wear and tear and inflammatory processes. Although the presence of synovitis and inflammation in OA joints may not be as pronounced as in inflammatory arthritis, it is still a significant factor in the development and progression of the disease. Understanding the causes, risk factors, symptoms, and management strategies for non-inflammatory knee osteoarthritis is crucial in providing optimal care and improving the quality of life for patients.
By identifying the various factors that contribute to the development of knee osteoarthritis, such as age, joint trauma, altered biomechanics, and obesity, healthcare professionals can work towards preventing and managing the condition effectively. Additionally, a comprehensive approach that combines lifestyle modifications, physical therapy, medications, injections, and surgical interventions can help alleviate symptoms and improve joint function in individuals with non-inflammatory knee osteoarthritis.
However, further research is needed to develop targeted therapies that can slow down the progression of the disease and provide long-term relief. By continued exploration of the inflammatory processes involved in non-inflammatory knee osteoarthritis, there is hope for the development of innovative treatments and interventions that can halt or even reverse the degenerative changes in the joints. This is an exciting area of research that holds the potential to significantly improve the lives of individuals affected by knee osteoarthritis and enhance their mobility and overall well-being.
FAQ
Is knee osteoarthritis considered non-inflammatory?
Yes, knee osteoarthritis is generally classified as non-inflammatory. However, recent studies suggest that there is a presence of synovitis, which is inflammation of the synovial membrane, in a significant proportion of patients with primary osteoarthritis.
What is the role of inflammation in osteoarthritis?
While inflammation in osteoarthritis is not as pronounced as in autoimmune diseases like rheumatoid arthritis, there is evidence of increased levels of inflammatory proteins and cytokines in the synovial fluid and tissues of osteoarthritis joints. This suggests that inflammation may contribute to the pathogenesis of osteoarthritis.
What are the causes and risk factors of non-inflammatory knee osteoarthritis?
Non-inflammatory knee osteoarthritis can be caused by various factors such as age, joint trauma, altered biomechanics, and obesity. Age-related changes in joint structures, previous joint injuries, abnormal joint mechanics, and excessive weight can all contribute to the development of non-inflammatory knee osteoarthritis.
What are the symptoms of non-inflammatory knee osteoarthritis?
The symptoms of non-inflammatory knee osteoarthritis include joint pain, stiffness, swelling, and a decreased range of motion.
How can non-inflammatory knee osteoarthritis be managed?
While there is no cure for osteoarthritis, there are several management strategies that can help alleviate symptoms and improve function. These may include lifestyle modifications, physical therapy, pain medications, intra-articular injections, and surgical interventions.
Leave a Reply