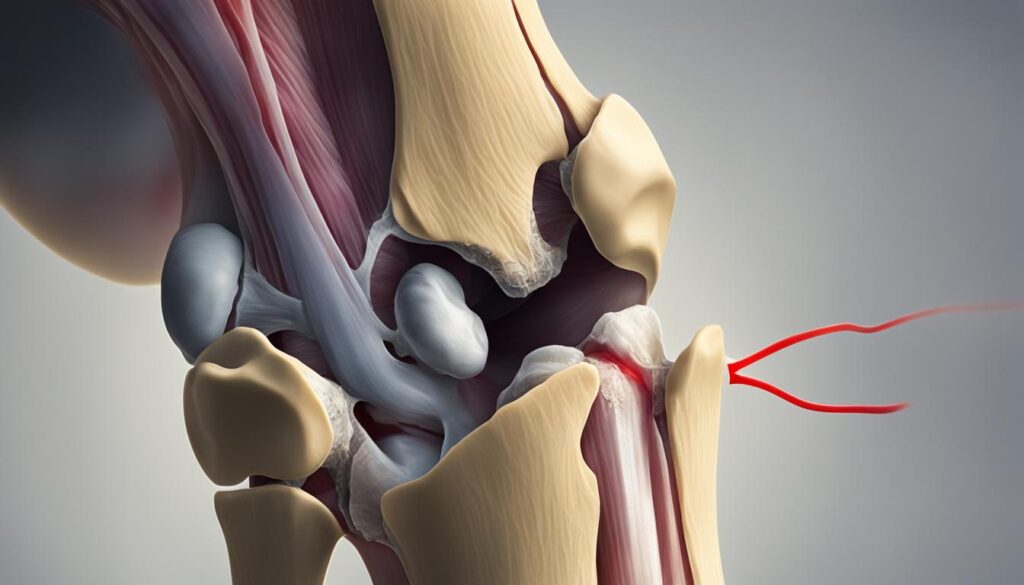
As we age, our bodies undergo various changes, and one condition that commonly affects our knees is osteoarthritis. Osteoarthritis in the knees, also known as wear-and-tear arthritis, occurs when the protective cartilage between the joints starts to deteriorate. This condition can cause pain, swelling, stiffness, and decreased mobility, making it challenging to carry out day-to-day activities.
For individuals with knees osteoarthritis, the question of when to stop working may arise. It’s essential to recognize that knee osteoarthritis doesn’t necessarily mean you have to cease all work or physical activity. In fact, staying active can be beneficial for managing the symptoms and maintaining overall joint health.
In this article series, we will explore the various aspects of knees osteoarthritis: its causes, symptoms, diagnosis, and treatment options. We will also discuss the impact of running on knee osteoarthritis and ways to manage the condition while engaging in exercise. Our goal is to provide comprehensive information that will help you make informed decisions about your health and well-being.
Remember, the information provided here is not intended to replace professional medical advice. It is always essential to consult with a healthcare professional to determine the best course of action for your specific condition. Together, we can navigate through knee osteoarthritis and find ways to manage it effectively, allowing you to live an active and fulfilling life.
Causes and Risk Factors of Knee Osteoarthritis
Understanding the causes and risk factors of knee osteoarthritis can help us better comprehend this prevalent condition and its impact on individuals. While knee osteoarthritis can be influenced by various factors, there are certain primary causes and risks to be aware of.
Primary Causes
The most common cause of knee osteoarthritis is age. As we age, the natural healing ability of cartilage decreases, making it more susceptible to wear and tear. Therefore, it is common for older individuals to develop knee osteoarthritis.
Risk Factors
In addition to age, several other risk factors contribute to the development of knee osteoarthritis. These include:
- Being overweight: Excessive weight puts additional stress on the knee joints, accelerating the wear and tear of cartilage.
- Heredity: Some individuals have a genetic predisposition to developing osteoarthritis, making them more susceptible to the condition.
- Gender: Women are more likely to develop knee osteoarthritis compared to men.
- Repetitive stress injuries: Certain occupations or activities that involve repetitive stress on the knees, such as construction work or professional sports, can increase the risk of developing knee osteoarthritis.
- Participation in high-impact sports: Sports that involve jumping, running, or sudden changes in direction can contribute to knee injuries, potentially leading to osteoarthritis over time.
- Other illnesses: Some medical conditions, such as rheumatoid arthritis and metabolic disorders, may heighten the risk of knee osteoarthritis.
By understanding these causes and risk factors, we can develop a more comprehensive approach to preventing and managing knee osteoarthritis. Awareness of these factors empowers us to make informed decisions regarding our lifestyle choices and healthcare plans.
| Cause/Risk Factor | Description |
|---|---|
| Age | The natural healing ability of cartilage decreases with age, making older individuals more prone to knee osteoarthritis. |
| Weight | Excessive weight places additional stress on the knees, accelerating the wear and tear of cartilage. |
| Heredity | Genetic factors can increase an individual’s susceptibility to knee osteoarthritis. |
| Gender | Women are more likely to develop knee osteoarthritis compared to men. |
| Repetitive Stress Injuries | Certain occupations or activities that involve repetitive stress on the knees can contribute to the development of knee osteoarthritis. |
| High-Impact Sports | Participation in sports that involve jumping, running, or sudden changes in direction can increase the risk of knee osteoarthritis over time. |
| Other Illnesses | Medical conditions such as rheumatoid arthritis and metabolic disorders may heighten the risk of knee osteoarthritis. |
Quote:
“By understanding the causes and risk factors of knee osteoarthritis, we can take proactive measures to minimize its impact and maintain optimal joint health.”
Now that we have examined the causes and risk factors of knee osteoarthritis, let us delve into the symptoms and diagnosis of this condition in the next section.
Symptoms and Diagnosis of Knee Osteoarthritis
Knee osteoarthritis can cause various symptoms that may affect your daily life and mobility. Recognizing these symptoms and seeking proper diagnosis is crucial for effective treatment. Common symptoms of knee osteoarthritis include:
- Pain that worsens with activity but improves with rest
- Swelling in the affected knee
- Stiffness, especially in the morning or after periods of inactivity
- Decreased mobility and difficulty bending or straightening the knee
- Creaking or grinding sounds (known as crepitus) when moving the knee
These symptoms can vary in severity and may worsen over time. If you experience any of these symptoms, it is important to consult with a healthcare professional for a proper diagnosis.
To diagnose knee osteoarthritis, a doctor will typically begin by performing a physical examination of the affected knee. During the exam, the doctor will assess the range of motion, stability, and strength of the knee joint. They may also inquire about your medical history and ask detailed questions about your symptoms.
In addition to the physical exam, imaging tests such as X-rays or MRIs may be ordered to assess the extent of cartilage damage and rule out other conditions. X-rays can reveal joint space narrowing, osteophyte formation (bone spurs), and other degenerative changes associated with osteoarthritis. MRIs provide a more detailed view of the soft tissues and can help determine the severity of cartilage damage.
In some cases, blood tests may be done to rule out other conditions that could be causing the knee pain, such as rheumatoid arthritis or gout.
Effective diagnosis of knee osteoarthritis is essential for developing an appropriate treatment plan. By accurately identifying the condition, healthcare professionals can recommend targeted interventions to alleviate pain, improve mobility, and enhance overall quality of life.
| Symptom | Description |
|---|---|
| Pain | Worsens with activity Improves with rest |
| Swelling | Puffiness or fluid accumulation In or around the knee joint |
| Stiffness | Especially in the morning Or after periods of inactivity |
| Decreased mobility | Difficulty bending or straightening the knee Limited range of motion |
| Creaking sounds | Grinding or popping noises When moving the knee |
Treatment Options for Knee Osteoarthritis
The primary goals of treating knee osteoarthritis are to relieve pain and improve mobility. There are several treatment options available that can help manage the symptoms and enhance the quality of life for individuals with knee osteoarthritis.
1. Weight Loss:
Weight loss plays a crucial role in reducing the stress on the knee joints. Excess weight can worsen the symptoms of knee osteoarthritis and accelerate joint damage. Losing weight through a combination of a healthy diet and regular exercise can significantly alleviate pain and improve mobility.
2. Exercise:
Exercise is a vital component of knee osteoarthritis treatment. Specific strengthening and stretching exercises can help improve joint stability, increase muscle strength, and enhance flexibility. Low-impact activities such as swimming, cycling, and walking are recommended as they minimize stress on the knee joint.
3. Medications:
In many cases, pain relievers and anti-inflammatory medications are prescribed to manage pain and reduce joint inflammation. Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen and naproxen sodium can provide temporary relief. Stronger prescription medications may be recommended for severe pain.
4. Injections:
Injections of corticosteroids or hyaluronic acid can be administered directly into the knee joint to reduce pain and inflammation. Corticosteroid injections provide rapid relief, while hyaluronic acid injections help lubricate the joint, improving mobility and reducing friction between the bones.
5. Alternative Therapies:
Alternative therapies such as topical creams, acupuncture, or transcutaneous electrical nerve stimulation (TENS) may also be considered as part of the treatment plan. These therapies can help reduce pain and improve physical function in some individuals.
6. Braces:
The use of braces or knee sleeves can provide support and stability to the affected knee. Braces can help offload the pressure from the damaged areas, reduce pain, and improve overall function.
7. Physical and Occupational Therapy:
Physical and occupational therapy can play a significant role in treating knee osteoarthritis. These therapies involve targeted exercises, manual therapy techniques, and assistive devices to improve joint function, enhance mobility, and provide education on proper body mechanics to prevent further joint damage.
8. Surgery:
In cases where conservative treatments fail to provide adequate relief, surgical interventions may be necessary. Arthroscopy, osteotomy, or joint replacement surgery may be recommended based on the severity of the condition and the individual’s overall health. Surgical interventions aim to repair or replace damaged joint components and restore normal function.
Comparison of Knee Osteoarthritis Treatment Options
| Treatment Option | Description | Advantages | Disadvantages |
|---|---|---|---|
| Weight Loss | Achieving a healthy weight through diet and exercise. | Reduces pressure on the knee joint, improves mobility. | Requires long-term commitment, may be challenging for some individuals. |
| Exercise | Specific strengthening and stretching exercises. | Improves joint stability, increases muscle strength. | May cause discomfort initially, needs consistency for long-term benefits. |
| Medications | Pain relievers and anti-inflammatory drugs. | Provides temporary relief, reduces joint inflammation. | Potential side effects, not a long-term solution. |
| Injections | Corticosteroid or hyaluronic acid injections into the knee joint. | Provides rapid pain relief, improves joint lubrication. | Temporary relief, may require multiple injections. |
| Alternative Therapies | Topical creams, acupuncture, or TENS for pain management. | Non-invasive options, may reduce pain and improve function. | Effectiveness varies, may not work for everyone. |
| Braces | Supportive devices to stabilize the knee joint. | Offers support, offloads pressure from damaged areas. | May restrict mobility, not suitable for all types of knee osteoarthritis. |
| Physical and Occupational Therapy | Targeted exercises and manual therapies. | Improves joint function, enhances mobility. | Requires regular sessions, commitment to long-term exercises. |
| Surgery | Arthroscopy, osteotomy, or joint replacement. | Repairs or replaces damaged joint components. | Can be invasive, involves recovery and potential risks. |
Running and Knee Osteoarthritis
Contrary to popular belief, running does not cause knee osteoarthritis. In fact, long-term studies have shown that running can have a positive impact on knee health and decrease the risk of hip and knee replacement compared to other forms of exercise.
Research has indicated that sedentary individuals have a higher incidence of knee osteoarthritis compared to recreational runners. This is because running helps to strengthen the muscles around the knee joint, support joint stability, and improve overall joint function.
“Running can be a beneficial activity for individuals with knee osteoarthritis. It helps to strengthen the muscles around the knee joint, maintain joint stability, and promote overall joint health.” – Dr. Sarah Johnson, Orthopedic Specialist.
However, it is important for individuals with knee osteoarthritis to listen to their bodies and take precautions when incorporating running into their exercise routine. Starting slowly and gradually increasing intensity can help minimize the risk of aggravating the condition.

During running, it’s crucial to pay attention to any pain or discomfort in the knees. If there is persistent pain, it’s recommended to consult with a healthcare professional for further evaluation and guidance.
In summary, running can actually have a positive impact on knee osteoarthritis by improving joint stability and reducing the risk of joint replacement. However, it is important to approach running with caution, listen to your body, and seek appropriate medical advice if needed.
Managing Knee Osteoarthritis During Exercise
When it comes to managing knee osteoarthritis during exercise, there are several key considerations to keep in mind. By understanding proper techniques and making the right choices, individuals can effectively manage their knee pain and continue to engage in physical activity.
Start Slow and Gradually Increase Intensity
For people with knee osteoarthritis, it’s essential to start any exercise program slowly and gradually increase intensity over time. This approach allows the body to adapt to the demands of exercise, reducing the risk of exacerbating knee pain or causing further damage. By pacing yourself and listening to your body, you can find a balance that works for you.
Distinguish Between Normal Muscle Soreness and Knee Pain
It’s important to distinguish between normal muscle soreness and knee pain associated with osteoarthritis. Muscle soreness is a common result of exercise and usually subsides within a day or two. On the other hand, knee pain related to osteoarthritis tends to persist and may worsen with certain movements. If you experience prolonged or worsening knee pain, it’s crucial to seek medical advice to determine the appropriate course of action.
Choose Proper Footwear
Selecting the right footwear is crucial for managing knee osteoarthritis during exercise. Shoes that provide adequate support and cushioning can help reduce impact on the knees and minimize discomfort. It is recommended to consult with a specialist at a running shoe store who can assess your gait and recommend the most suitable shoes for your needs.
Consider Other Factors
Aside from footwear, other factors such as running form, surface, and training load should be taken into consideration. Improper running form can put additional stress on the knees, so it’s important to maintain good posture and practice proper running techniques. Running on softer surfaces, such as grass or trails, can help reduce impact compared to concrete or asphalt. Additionally, managing training load by incorporating rest days and gradually increasing mileage can also prevent overuse injuries and minimize knee pain.
Rest and Recover
If knee pain worsens during exercise, it is crucial to listen to your body and take appropriate rest periods. Pushing through the pain can lead to further injury and may exacerbate osteoarthritis symptoms. Allowing ample time for rest and recovery enables the knees to heal and reduces the risk of long-term damage.
Track Your Progress
Keeping a journal to track progress and guide future workouts can be a helpful tool in managing knee osteoarthritis during exercise. By recording your activities, pain levels, and any modifications made, you can identify patterns and make adjustments accordingly. This self-reflection can provide valuable insights into what works best for your body and help you make informed decisions about your exercise routine.
Conclusion
Knee osteoarthritis is a prevalent condition that affects many individuals, causing discomfort and limitations in daily activities. However, it does not mean that you have to give up working or exercising entirely. With the right approach to management, you can still lead an active and fulfilling life despite knee osteoarthritis.
Our recommended strategies for managing knee osteoarthritis include weight loss, exercise, pain management techniques, and, in some cases, surgical interventions. By working closely with healthcare professionals, you can determine the most suitable treatment plan for your specific condition, ensuring optimal results.
Remember to listen to your body and pace yourself during activities. It’s essential to strike a balance between staying active and avoiding excessive strain on your knees. By making informed choices and following a personalized treatment plan, you can effectively manage knee osteoarthritis and enjoy a fulfilling lifestyle.
FAQ
Should I stop working if I have knee osteoarthritis?
Whether or not you should stop working with knee osteoarthritis depends on the severity of your symptoms and the demands of your job. It is important to consult with your healthcare professional to determine if any work modifications or occupational restrictions are necessary.
What are the causes and risk factors of knee osteoarthritis?
The most common cause of knee osteoarthritis is age, as the ability of cartilage to heal decreases with age. Other risk factors include being overweight, hereditary factors, gender (women are more likely to develop osteoarthritis), repetitive stress injuries from certain occupations, and participation in high-impact sports. Certain illnesses such as rheumatoid arthritis and metabolic disorders may also increase the risk of knee osteoarthritis.
What are the symptoms and how is knee osteoarthritis diagnosed?
Common symptoms of knee osteoarthritis include pain that worsens with activity but improves with rest, swelling, stiffness (especially in the morning or after periods of inactivity), decreased mobility, and creaking sounds in the knee. To diagnose knee osteoarthritis, a doctor will perform a physical exam, take a medical history, and may order X-rays or MRIs to assess the extent of cartilage damage. Blood tests may be done to rule out other conditions that could be causing the pain.
What are the available treatment options for knee osteoarthritis?
The primary goals of treating knee osteoarthritis are to relieve pain and improve mobility. Treatment options include weight loss, exercise (both strengthening and stretching exercises), pain relievers and anti-inflammatory drugs, injections of corticosteroids or hyaluronic acid into the knee, alternative therapies such as topical creams or acupuncture, the use of braces, and physical and occupational therapy. In cases where conservative treatments fail, surgery such as arthroscopy, osteotomy, or joint replacement may be recommended.
Does running cause knee osteoarthritis?
Contrary to popular belief, running does not cause knee osteoarthritis. In fact, long-term studies have shown that running can decrease the risk of hip and knee replacement compared to other forms of exercise. Sedentary individuals have a higher incidence of knee osteoarthritis compared to recreational runners. However, elite competitive runners may have a higher risk of knee osteoarthritis. It is important for individuals with knee osteoarthritis to listen to their bodies, start slowly, and pay attention to any pain or discomfort during running.
How can I manage knee osteoarthritis during exercise?
People with knee osteoarthritis should start any exercise program slowly and gradually increase intensity. It is important to distinguish between normal muscle soreness and knee pain associated with osteoarthritis. Proper footwear is crucial, and consulting with a specialist at a running shoe store is recommended. Other factors such as running form, surface, and training load should also be considered. If pain worsens during exercise, it is important to rest and allow the knees to recover. Keeping a journal to track progress and guide future workouts can be helpful.
Can I still lead an active life with knee osteoarthritis?
Knee osteoarthritis is a common condition that can cause pain, stiffness, and decreased mobility in the knee joint. However, it is not a reason to stop working or exercising altogether. With proper management, including weight loss, exercise, pain management strategies, and, in some cases, surgery, individuals with knee osteoarthritis can continue to lead active and fulfilling lives. It is important to consult with healthcare professionals and listen to your body to determine the best treatment plan for your specific condition.

Leave a Reply