This is evident from a recent study published in the journal JAMA network openedResearchers in Canada investigated whether coronavirus disease 2019 (COVID-19) patients with immune-mediated inflammatory diseases (IMIDs) were at higher risk of experiencing venous thromboembolism after recovery from severe acute respiratory syndrome coronavirus 2 (SARS-CoV- 2) infections compared to COVID-19 patients without IMIDs.
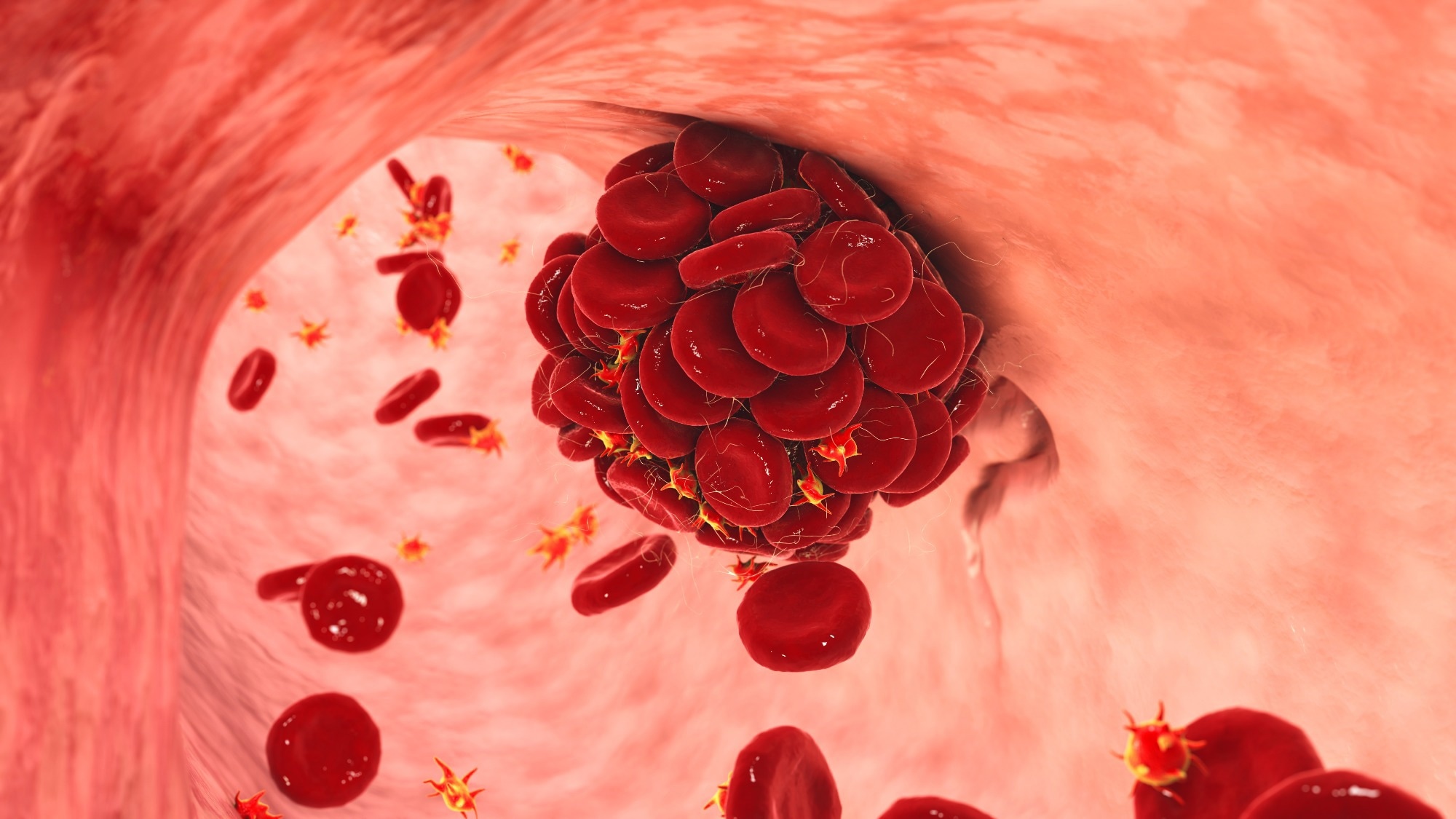 Study: Venous thromboembolism after COVID-19 infection in people with and without immune-mediated inflammatory diseases. Image credits: Kateryna Kon / Shutterstock
Study: Venous thromboembolism after COVID-19 infection in people with and without immune-mediated inflammatory diseases. Image credits: Kateryna Kon / Shutterstock
Background
Immune-mediated inflammatory diseases are heterogeneous chronic diseases resulting from an abnormally activated immune system. Approximately 5% to 7% of the population of the Western world is affected by IMIDs, and individuals with IMIDs have a higher risk of venous thromboembolism compared to individuals without IMIDs. Rheumatoid arthritis, multiple sclerosis, vasculitis, inflammatory bowel disease, and psoriasis are IMIDs known to increase the risk of venous thromboembolism.
The inflammation in IMID patients causes platelet abnormalities, endothelial dysfunction, fibrinolysis disorders, and abnormal activation of clotting factors. Recent evidence also indicates that the widespread inflammation and endothelial dysfunction caused by COVID-19 is associated with a higher risk of venous thromboembolism and multi-organ failure in patients who have recovered from moderate to severe SARS-CoV-2 infections. However, whether COVID-19 increases the risk of venous thromboembolism in patients with IMIDs remains unknown.
About the study
In the current study, the researchers used population-based healthcare data from Ontario, Canada, to evaluate whether the risk and incidence of venous thromboembolism were higher in individuals with IMIDs who had recovered from COVID-19 compared to COVID-19 . patients without IMIDs.
The data includes all interactions Ontario residents with valid health cards had with the health care system, including emergency room visits, hospital admissions, outpatient surgeries and single-day hospital admissions. In addition, physician billings for all patient interactions were included in the data. The administrative health information was also linked to databases containing demographic information and data on COVID-19 testing and vaccination status.
In the retrospective matched cohort analysis, researchers matched individuals who had IMIDs and tested positive for COVID-19 with up to five individuals who tested positive for COVID-19 but did not have IMIDs. Controls were compared based on factors such as age, gender, urban or rural residence, and average income quantile of the neighborhood. Individuals with a diagnosis of malignant neoplasm five years after a positive COVID-19 test were excluded from the study.
Positive cases of COVID-19 were identified based on polymerase chain reaction (PCR) results, while individuals with IMIDs were identified based on physician billings, records of endoscopy procedures, and medication prescriptions specific to IMIDs. Data on hospital admissions and emergency department visits were used to identify events of venous thromboembolism. The primary outcome examined was venous thromboembolism of any type, with secondary outcomes including pulmonary embolism and deep venous thrombosis.
A modified Charlson Comorbidity Index was used to include comorbidities such as diabetes, chronic obstructive pulmonary disease, or congestive heart failure before the positive diagnosis of COVID-19. Individuals with at least two vaccination doses before positive diagnosis of COVID-19 were considered vaccinated. In addition, socio-demographic factors such as residential areas in urban or rural areas, gender, age, socio-economic status and death before the conclusion of follow-up were also taken into account during the analysis.
Results
The findings suggested that individuals with IMIDs did not have a significantly higher risk of venous thromboembolism after recovery from SARS-CoV-2 infections compared to individuals without IMIDs. Among the 28,440 individuals with IMIDs included in the study, the incidence of venous thromboembolism was 2.64 per 100,000 person-days, while in the matched cohorts of individuals without IMIDs it was 2.18 per 100,000 person-days.
However, when the analysis was not adjusted for comorbidities, those with IMIDs had a greater risk of venous thromboembolism after recovery from COVID-19 than those without IMIDs. Furthermore, findings were similar when the risk of deep venous thrombosis and pulmonary embolism was examined separately.
The presence of other comorbidities was found to confound the association between venous thromboembolism and IMIDs after SARS-CoV-2 infections. These findings highlight the need for physicians to consider factors such as comorbidities and individual risk factors when prescribing venous thromboembolism prophylactics to IMID patients who have recovered from COVID-19.
Conclusions
Overall, the findings reported that patients with IMIDs are not at greater risk of venous thromboembolism after SARS-CoV-2 infections compared to COVID-19 patients without IMIDs. However, some comorbidities may confound the association between IMIDs and venous thromboembolism associated with COVID-19, and physicians should consider individual risk factors when treating IMID patients for COVID-19 complications.
Magazine reference:
- Khan, R., Ellen, K. M., Tang, F., James, Widdifield, J., McCurdy, J. D., Kaplan, GG, & Benchimol, E. I. (2023). Venous thromboembolism after COVID-19 infection in people with and without immune-mediated inflammatory diseases. JAMA network opened, 6(10), e2337020–e2337020. https://doi.org/10.1001/jamanetworkopen.2023.37020

Leave a Reply