Welcome to our comprehensive guide on osteoarthritis. In this article, we will delve into the causes, risk factors, symptoms, and management options for this degenerative joint disease. Osteoarthritis is a condition that affects millions of people worldwide, causing pain, stiffness, and limited mobility in various joints. By understanding the factors that contribute to the development of osteoarthritis, we can take proactive steps to prevent its onset and effectively manage its symptoms.
Osteoarthritis is influenced by various factors, including aging, obesity, joint injuries, repetitive movements, and genetic predisposition. While the exact trigger for the breakdown of joint tissues is unknown, these factors can increase the risk of developing osteoarthritis. The symptoms of osteoarthritis can significantly impact daily activities and lead to muscle weakness and fatigue. However, there are various treatment options available to manage the condition and improve quality of life.
Throughout this guide, we will provide valuable insights into the causes, progression, and management of osteoarthritis. We will explore the importance of early diagnosis, effective treatment options, and lifestyle modifications that can help individuals live well with osteoarthritis. Whether you are someone living with osteoarthritis or seeking information for a loved one, our goal is to provide you with the knowledge and resources you need to navigate this condition with confidence.
Stay tuned for the upcoming sections where we will delve deeper into the specifics of what happens in osteoarthritis, who is most at risk, the symptoms to look out for, the causes of the condition, how it is diagnosed, and the various treatment options available. By the end of this guide, you will have a comprehensive understanding of osteoarthritis and the tools to effectively manage it.
What happens in osteoarthritis?
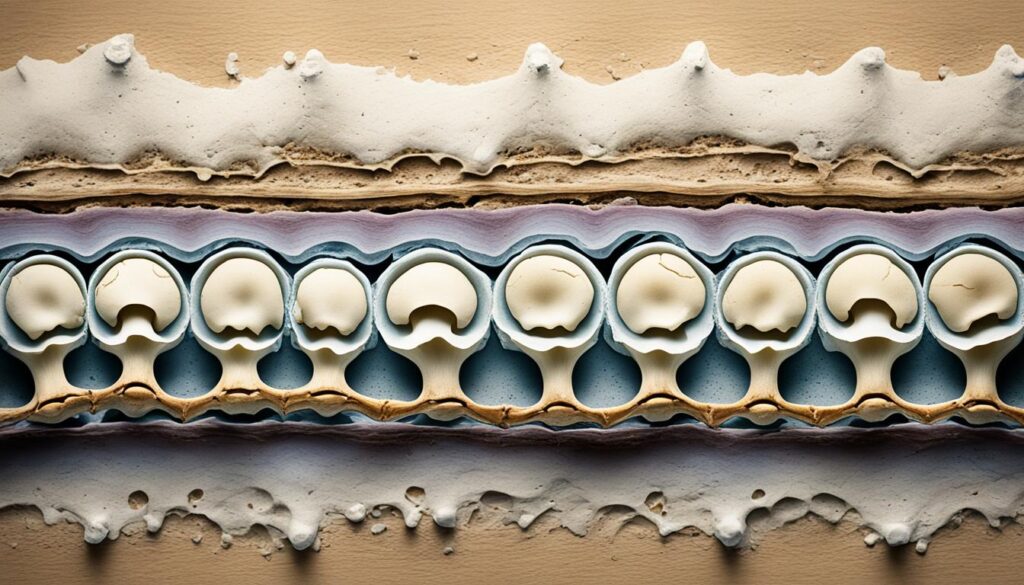
In osteoarthritis, the tissues in the joint undergo a gradual breakdown, leading to various symptoms and complications. The joint is composed of different structures, including cartilage, tendons, ligaments, synovium, and bone. Over time, these tissues deteriorate, resulting in joint damage and dysfunction.
The breakdown of cartilage, the smooth and protective surface covering the ends of bones, is a hallmark of osteoarthritis. Cartilage loss causes bones to rub against each other, leading to pain, swelling, and stiffness in the affected joint. This can significantly impact an individual’s mobility and overall quality of life.
Soft tissue damage is another consequence of osteoarthritis. Tendons, ligaments, and the synovium surrounding the joint may become inflamed and weakened. This can further exacerbate joint pain and limit joint motion, making it difficult for individuals to perform daily activities.
The structural changes in the joint can also result in shape alterations. Osteoarthritis can lead to joint shape changes, such as bone spurs or osteophytes developing along the edges of the joint. These bony growths can cause additional pain and further restrict joint movement.
The Impact of Joint Damage
Joint damage in osteoarthritis can cause several complications. The damaged joint may experience chronic pain, which can be severe and debilitating. Joint pain may worsen with movement or weight-bearing activities, making it challenging to perform everyday tasks.
Joint swelling is another common symptom in osteoarthritis. The inflammation in the joint can cause the accumulation of fluid, leading to swelling and discomfort. Swollen joints can become tender to the touch and may feel warm.
The loss of joint function due to osteoarthritis can result in limited mobility. Stiffness and reduced range of motion make it difficult to bend, straighten, or rotate the affected joint fully. This can impact an individual’s ability to perform essential movements, such as walking, climbing stairs, or grasping objects.
Osteoarthritis can significantly affect individuals’ daily lives, making it essential to effectively manage the condition and seek appropriate treatment options. By understanding the mechanisms behind osteoarthritis and its impact on joint health, individuals can take proactive steps to alleviate symptoms and enhance their overall well-being.
| Effects of Osteoarthritis | Description |
|---|---|
| Joint pain | Chronic pain in the affected joint, worsened by movement or weight-bearing activities. |
| Joint swelling | Inflammation in the joint causing the accumulation of fluid, resulting in swelling and tenderness. |
| Loss of joint function | Stiffness and restricted range of motion, impacting daily activities and mobility. |
Who gets osteoarthritis?
Osteoarthritis can affect people of all ages, but its prevalence increases with age. Older individuals are more susceptible to developing osteoarthritis due to the natural wear and tear that occurs in the joints over time. Moreover, women, especially after menopause, have a higher risk of developing osteoarthritis compared to men.
However, it is noteworthy that younger individuals can also develop osteoarthritis. In these cases, the disease is often a result of various factors, including:
- Joint injuries: A history of joint injuries or trauma can contribute to the development of osteoarthritis at a younger age.
- Abnormal joint structure: Some individuals may have congenital or acquired joint abnormalities that increase their susceptibility to osteoarthritis.
- Genetic defects: Certain genetic defects in joint cartilage can predispose younger individuals to osteoarthritis.
Additionally, there are several other risk factors for osteoarthritis that apply to individuals of all age groups. These include:
- Aging: As mentioned earlier, the risk of developing osteoarthritis increases with age.
- Obesity: Being overweight or obese puts extra stress on the joints, increasing the risk of osteoarthritis.
- Overuse of joints: Excessive and repetitive use of joints, such as in certain occupations or sports activities, can contribute to joint deterioration and osteoarthritis.
- Joint deformities: Structural abnormalities or misalignment of joints can contribute to the development of osteoarthritis.
- Family history: Having a family history of osteoarthritis can increase an individual’s risk of developing the disease.
It is important to recognize the various risk factors for osteoarthritis, as this can help individuals take preventive measures and make informed lifestyle choices to reduce the likelihood of developing the condition.

Symptoms of osteoarthritis
In osteoarthritis, the symptoms develop gradually and can vary depending on the affected joints. Common symptoms include:
- Joint pain in osteoarthritis: Individuals with osteoarthritis may experience pain in the joints, which can range from mild discomfort to severe aches.
- Joint stiffness in osteoarthritis: Stiffness in the joints, especially after periods of rest or inactivity, is a common symptom.
- Joint changes in osteoarthritis: Osteoarthritis can lead to changes in the shape and structure of the joints, such as bony enlargements in the hands or grinding noises in the knees.
- Joint swelling in osteoarthritis: Swelling around the joints can occur due to inflammation and fluid accumulation.
- Limited joint movement in osteoarthritis: As the condition progresses, individuals may experience limited mobility and difficulty moving the affected joints.
It’s important to note that the symptoms of osteoarthritis can vary from person to person and depend on the severity of the condition. Some individuals may experience mild symptoms that do not significantly impact their daily lives, while others may experience more severe symptoms that limit their ability to perform everyday activities.
The Impact of Osteoarthritis on Daily Life
Osteoarthritis can have a significant impact on an individual’s daily life. The joint pain, stiffness, and limited movement can make it challenging to perform simple tasks and engage in physical activities. Daily activities such as walking, climbing stairs, and even holding objects can become difficult and painful. Osteoarthritis can also affect sleep quality, leading to fatigue and reduced productivity during the day.
Managing the symptoms of osteoarthritis requires a multi-faceted approach that includes medication, physical therapy, lifestyle modifications, and assistive devices. By implementing a comprehensive treatment plan, individuals can alleviate pain, improve joint function, and enhance their overall quality of life.
Causes of osteoarthritis
Osteoarthritis, a degenerative joint disease, can be caused by various factors that contribute to the deterioration and structural changes within the joint. While the exact cause of osteoarthritis is unknown, several triggers have been identified:
- Aging: The risk of developing osteoarthritis increases with age. As we get older, the natural wear and tear on our joints can lead to cartilage breakdown and joint stiffness.
- Overweight and obesity: Excess weight puts additional stress on the joints, particularly the knees and hips, increasing the likelihood of developing osteoarthritis.
- Joint injury: Trauma to the joint, such as fractures or ligament tears, can disrupt the normal structure of the joint and accelerate cartilage degeneration.
- Overuse of joints: Repetitive movements or activities that put excessive stress on the joints, such as those performed in certain occupations or sports, can contribute to the development of osteoarthritis.
- Joint abnormalities: Structural abnormalities in the joint, such as misaligned joints or abnormal cartilage formation, can increase the risk of osteoarthritis.
- Family history: Individuals with a family history of osteoarthritis are more likely to develop the condition. Genetic factors may play a role in the development and progression of the disease.
Osteoarthritis is not solely attributed to wear and tear on the joints; it involves complex changes in the joint tissues and inflammation. Understanding the causes and triggers of osteoarthritis is crucial for prevention, early detection, and effective management of the disease.
| Cause | Description |
|---|---|
| Aging | The natural process of aging can contribute to joint degeneration and the development of osteoarthritis. |
| Overweight and Obesity | Excess weight puts stress on the joints, increasing the risk of cartilage deterioration and osteoarthritis. |
| Joint Injury | Acute injuries, such as fractures or ligament tears, can disrupt the joint structure and accelerate cartilage breakdown. |
| Overuse of Joints | Repetitive activities or occupations that strain the joints can contribute to the development of osteoarthritis. |
| Joint Abnormalities | Structural abnormalities, such as misaligned joints or abnormal cartilage formation, can increase the risk of osteoarthritis. |
| Family History | Having a family history of osteoarthritis increases the likelihood of developing the condition. |
By understanding the causes of osteoarthritis, individuals can take proactive steps to reduce their risk and manage the disease effectively. It is important to prioritize joint health through weight management, proper nutrition, regular exercise, and injury prevention strategies.
Diagnosis of osteoarthritis
Diagnosing osteoarthritis involves a comprehensive evaluation that includes a detailed medical history, a physical examination, and specific lab tests. Our healthcare professionals are trained to assess your symptoms, medical history, joint pain, stiffness, and mobility to determine the presence of osteoarthritis.
A thorough medical history is crucial for understanding your symptoms and identifying any risk factors or underlying conditions that may contribute to osteoarthritis. This information helps us develop a personalized treatment plan that addresses your specific needs.
During the physical examination, our healthcare professionals will examine the affected joints, assessing their range of motion, tenderness, and any signs of swelling or deformity. This examination provides valuable insights into the severity and progression of osteoarthritis in your joints.
In some cases, lab tests may be ordered to support the diagnosis of osteoarthritis. These tests can help rule out other conditions with similar symptoms and provide additional information about the progression of the disease. Lab tests may include analyzing fluid extracted from the affected joint through a procedure called joint aspiration.
Imaging tests such as X-rays and MRI scans are commonly used to visualize joint and bone damage associated with osteoarthritis. X-rays can show changes in bone density, joint space narrowing, and the presence of osteophytes or bone spurs. MRI scans provide detailed images of soft tissues, helping to identify cartilage damage and other structural abnormalities.
Summary of Diagnostic Methods for Osteoarthritis
| Diagnostic Method | Description |
|---|---|
| Medical History | A detailed evaluation of your symptoms, risk factors, and underlying medical conditions. |
| Physical Examination | A comprehensive assessment of joint function, mobility, and signs of inflammation or deformity. |
| Lab Tests | Analysis of fluid extracted from the affected joint to rule out other conditions. |
| X-ray | Radiographic imaging that can reveal bone damage, joint space narrowing, and osteophytes. |
| MRI | Detailed imaging of soft tissues, providing insights into cartilage damage and structural abnormalities. |
By combining these diagnostic methods, we can accurately diagnose osteoarthritis and develop a tailored treatment plan to manage your symptoms and improve your quality of life.
Treatment of osteoarthritis
In managing osteoarthritis, there are various treatment options available that can help alleviate symptoms and enhance overall quality of life. These options encompass a range of approaches, including medication, non-drug therapies, physical therapies, assistive devices, and joint surgery.
Medication for Osteoarthritis
In many cases, medication can be an effective method of pain management for osteoarthritis. Commonly prescribed medications include:
- Pain relievers: Over-the-counter pain relievers, such as acetaminophen, can provide temporary relief from mild to moderate pain.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs, like ibuprofen or naproxen sodium, can reduce pain and inflammation. These medications are available both over-the-counter and by prescription.
- Corticosteroid injections: For individuals with moderate to severe pain, corticosteroid injections directly into the affected joint can offer significant relief by reducing inflammation.
Non-Drug Therapies for Osteoarthritis
Non-drug therapies focus on managing osteoarthritis symptoms without relying on medication. These therapies include:
- Exercise: Regular physical activity, such as low-impact exercises and stretching, can help strengthen the muscles around the affected joint, improve range of motion, and alleviate pain.
- Weight loss: For individuals who are overweight or obese, losing weight can help reduce the stress placed on the joints, leading to decreased pain and improved mobility.
- Physical therapies: Techniques like heat or cold therapy, transcutaneous electrical nerve stimulation (TENS), and ultrasound therapy can all contribute to pain relief and improved joint function.
- Assistive devices: The use of assistive devices like braces, canes, or shoe inserts can help support the joint, reduce stress, and improve stability and mobility.
Joint Surgery for Osteoarthritis
In cases where non-surgical approaches do not provide sufficient relief, joint surgery may be considered. Common surgical options include:
- Joint fusion: In this procedure, the damaged joint surfaces are fused together, reducing pain and improving joint stability. However, joint fusion limits joint mobility.
- Joint replacement: Joint replacement surgery involves replacing the damaged joint with a prosthesis made of metal, plastic, or ceramic. This option can significantly relieve pain and restore joint function.
It is important for individuals with osteoarthritis to work closely with their healthcare providers to develop a personalized treatment plan that suits their specific needs and preferences. By utilizing a combination of these treatment options, individuals can effectively manage their symptoms, reduce pain, and enjoy an improved quality of life despite the challenges presented by osteoarthritis.
Conclusion
Osteoarthritis is a common degenerative joint disease that can greatly impact our daily lives. While the exact cause is still under study, several factors contribute to its development. It is crucial to understand the symptoms, risk factors, and treatment options available for managing osteoarthritis. Early diagnosis and the implementation of appropriate management strategies can help us effectively manage pain, increase mobility, and maintain an overall high quality of life.
Lifestyle modifications, including regular exercise, weight management, medication, physical therapies, and the use of assistive devices, all play a crucial role in managing osteoarthritis. By taking proactive steps to prevent and manage this condition, we can live well with osteoarthritis and minimize its impact on our daily lives.
Remember, prevention is key. While osteoarthritis cannot be entirely prevented, adopting a healthy lifestyle, maintaining a nutritious diet, and avoiding joint injuries can help reduce the risk of developing this condition. By being proactive and implementing effective management strategies, we can enhance our well-being and effectively navigate living with osteoarthritis.
FAQ
What are the causes of osteoarthritis?
The exact cause of osteoarthritis is unknown, but factors such as aging, obesity, joint injuries, repetitive movements, and genetic predisposition can increase the risk of developing the disease.
What happens in osteoarthritis?
Osteoarthritis is a degenerative joint disease where the tissues in the joint, including the cartilage, tendons, ligaments, synovium, and bone, gradually break down. This leads to pain, swelling, and loss of joint motion. The damage can affect all areas of the joint and may cause changes in the joint’s shape.
Who is at risk of developing osteoarthritis?
Osteoarthritis is most common in older individuals, but it can affect anyone. Risk factors include aging, obesity, joint injuries or surgeries, overuse of joints, joint deformities, and family history of osteoarthritis.
What are the symptoms of osteoarthritis?
The symptoms of osteoarthritis can vary, but they often include joint pain, stiffness, limited mobility, swelling, and changes in joint shape. The specific symptoms depend on the affected joints.
What are the causes of osteoarthritis?
Osteoarthritis can be caused by various factors such as aging, being overweight or obese, joint injuries or surgeries, overuse of joints, joint abnormalities, and a family history of osteoarthritis.
How is osteoarthritis diagnosed?
Osteoarthritis is diagnosed through a detailed medical history, physical examination, and specific lab tests. Imaging tests such as X-rays or MRI scans can also show joint and bone damage associated with osteoarthritis.
What are the treatment options for osteoarthritis?
There is no cure for osteoarthritis, but various treatment options can help manage symptoms. These include medication, physical therapy, exercise, weight management, and the use of assistive devices. In severe cases, joint surgery may be recommended.
How can osteoarthritis be managed?
Living with osteoarthritis involves managing symptoms through lifestyle modifications, such as exercise, weight management, and the use of medication, physical therapies, and assistive devices. Early diagnosis and appropriate management strategies can help individuals maintain their quality of life.

Leave a Reply