Have you ever wondered why simple movements like walking downstairs suddenly feel challenging? For many Americans, discomfort in the knee area during daily activities signals deeper joint concerns. Research shows this sensation often stems from pressure imbalances around the patella – a problem affecting 25% of adults at some point.
This type of joint issue can transform routine tasks into uncomfortable experiences. While some cases involve temporary strain, others may indicate conditions affecting cartilage alignment or soft tissue health. Factors like repetitive motion, muscle imbalances, or previous injuries frequently play roles.
We’ve designed this guide to help you understand what your body might be communicating. From practical prevention strategies to recognizing when professional consultation becomes essential, our approach combines medical insights with actionable advice. Let’s explore how to restore confidence in your movements.
Key Takeaways
- Knee discomfort during downward movements often relates to patellar tracking issues
- Daily activities like stair use can reveal early signs of joint stress
- Muscle strength and flexibility significantly impact knee function
- Persistent symptoms warrant evaluation by a healthcare provider
- Preventive measures can reduce recurrence of symptoms
- Treatment options range from physical therapy to targeted exercises
Understanding Knee Pain on Stair Descent
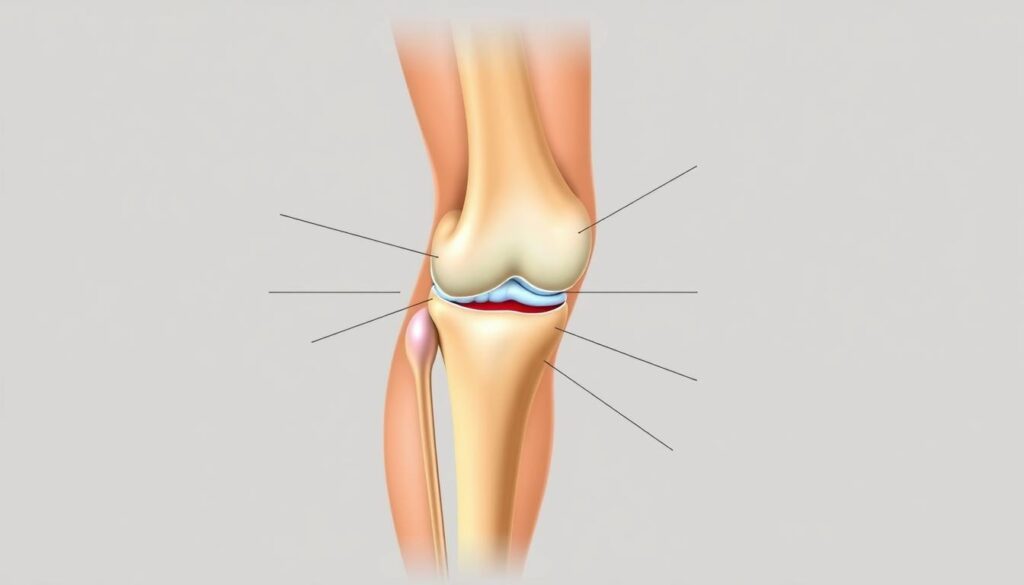
Navigating daily movements requires precise coordination between bones, muscles, and connective tissues. The knee joint acts as a sophisticated hinge, combining the femur, tibia, and patella with shock-absorbing cartilage. Quadriceps and hamstrings provide power while tendons anchor these muscles to the bone, creating smooth motion during activities like bending or stepping.

Overview of Knee Joint Function
This complex system distributes body weight across three main contact points. When functioning optimally, cartilage cushions each step and prevents friction. However, weakened thigh muscles or uneven pressure can disrupt this balance. Downward movements like stair navigation multiply force on the patella by up to 3.5 times body weight, according to biomechanical studies.
Common Symptoms and Signs
Early indicators often include:
- Grinding sensations during knee bends
- Morning stiffness that eases with movement
- Tenderness along the joint line
Many people notice discomfort first after prolonged sitting – a phenomenon called “theater sign.” This occurs because cartilage needs regular movement to maintain nutrient flow. Persistent symptoms during stair use suggest the need for professional evaluation to prevent progressive damage.
Recognizing Pain behind kneecap when descending stairs
Many active adults notice a specific type of joint discomfort that appears during downward movements. This sensation, often described as pressure or aching around the front knee area, frequently signals patellofemoral pain syndrome. Unlike general joint soreness, this condition specifically affects where the thigh bone meets the kneecap.
Definition and Key Characteristics
Patellofemoral pain syndrome develops when uneven forces strain the cartilage beneath the kneecap. Key identifiers include:
- Discomfort that worsens with repeated bending motions
- A sensation of joint “catching” during movement
- Tenderness around the edges of the kneecap
Research shows 40% of cases involve abnormal patella tracking during activity. Muscle weakness in the hips or thighs often contributes to this misalignment, creating excessive pressure on specific cartilage areas.
| Feature | General Knee Pain | Patellofemoral Discomfort |
|---|---|---|
| Primary Location | Entire joint area | Front and center behind kneecap |
| Common Triggers | Impact activities | Stair descent, squatting |
| Duration Patterns | Variable | Gradual onset over weeks |
When to Seek Professional Advice
Schedule an evaluation if symptoms persist beyond two weeks or limit daily activities. Medical guidance becomes crucial when experiencing:
- Swelling that doesn’t improve with rest
- Audible popping sounds during movement
- Difficulty bearing weight on the affected leg
The American Academy of Orthopaedic Surgeons recommends early intervention for patellofemoral issues. Proper diagnosis helps prevent long-term cartilage damage and guides effective treatment plans.
Exploring Underlying Causes and Contributing Factors
Understanding why knees protest during downward movements requires examining multiple factors. Four primary conditions often explain discomfort during stair navigation, each with distinct mechanisms and risk profiles.
Patellofemoral Pain Syndrome (Runner’s Knee)
This syndrome affects 22% of active adults, per Sports Health Journal. Misaligned kneecap movement irritates surrounding tissues, creating a dull ache. Muscle imbalances in hips or thighs often drive this abnormal patella tracking.
Chondromalacia Patella Considerations
Softened cartilage beneath the kneecap leads to sharp discomfort during bends. Unlike temporary strain, this condition involves progressive wear often seen in cyclists and gymnasts. Repeated friction from poor alignment accelerates cartilage breakdown.
Pes Anserine Bursitis and Osteoarthritis Insights
Inflammation near the inner knee (pes anserine bursitis) commonly stems from overuse in runners. Meanwhile, osteoarthritis wears down joint cushioning over time. Johns Hopkins research links every 10 lbs of excess weight to 36% increased knee stress during movement.
| Condition | Primary Cause | Key Risk Factors | Common Symptoms |
|---|---|---|---|
| Patellofemoral Syndrome | Kneecap misalignment | Sports participation, muscle weakness | Dull front-knee ache |
| Chondromalacia | Cartilage degeneration | Repetitive bending, prior injury | Grinding sensations |
| Osteoarthritis | Joint wear | Age, obesity, genetics | Morning stiffness |
While these conditions differ, they share preventable elements. Targeted strength training and activity modifications help manage symptoms across all diagnoses. Early intervention remains crucial for preserving joint function.
At-Home Treatments and Immediate Relief Strategies
Effective self-care methods can significantly improve joint comfort during recovery phases. We’ll guide you through proven techniques that reduce pain and support healing without requiring special equipment.
Step-by-Step Recovery Protocol
The RICE method remains a gold standard for acute symptom management. Studies show this approach can help reduce inflammation by up to 40% within 48 hours:
- Rest: Pause activities causing discomfort – even brief breaks prevent further strain
- Ice: Apply cold packs for 15-minute intervals to reduce swelling
- Compression: Use elastic bandages to stabilize the area without restricting circulation
- Elevation: Keep legs raised above heart level when resting
Over-the-counter NSAIDs like ibuprofen provide temporary relief when used as directed. Pair these with gentle muscle-stretching routines to maintain flexibility.
Adjust daily routines to avoid flare-ups. Swap stair use for elevator access temporarily. If symptoms persist beyond 72 hours despite these measures, consult a healthcare provider to rule out serious conditions.
| Treatment | Frequency | Expected Results |
|---|---|---|
| Ice Application | 3-4x daily | Reduced inflammation |
| Compression Wrap | Daytime use | Improved joint stability |
| Elevation | 2 hours daily | Faster fluid drainage |
The Role of Physical Therapy in Managing Knee Pain
Professional guidance transforms knee rehabilitation through science-backed strategies. Research shows 65% of patients report long-term improvement after completing structured therapy programs. These interventions address muscle imbalances and movement patterns that contribute to joint stress.
Effective Exercises and Strengthening Routines
Therapists design programs targeting specific weaknesses. Quadriceps strengthening using mini-squats improves patellar tracking. Hip stabilization drills with resistance bands enhance overall joint alignment.
Key routines include:
- Step-ups with controlled lowering
- Straight-leg raises to engage thigh muscles
- Clamshell exercises for hip abductor strength
A 12-week study in Journal of Orthopaedic Therapy found participants gained 30% more leg strength compared to self-guided workouts.
Manual Therapy and Taping Techniques
Hands-on methods complement exercise regimens. Soft tissue mobilization breaks down scar tissue while improving cartilage nutrition. Kinesiology tape applications provide external support during daily activities.
| Technique | Purpose | Frequency |
|---|---|---|
| Joint Mobilization | Restore kneecap movement | 2x weekly |
| Myofascial Release | Reduce muscle tightness | 3x weekly |
| Therapeutic Taping | Improve alignment | During activity |
Consistent therapy sessions help retrain movement patterns. This professional guidance ensures exercises match individual biomechanical needs for lasting results.
Lifestyle Factors and Long-Term Pain Reduction Strategies
Sustaining joint health requires more than temporary fixes – it demands thoughtful daily choices. Research confirms that 60% of chronic joint issues improve through consistent lifestyle adjustments. Let’s explore sustainable methods to protect your mobility.
Weight Management and Joint Support
Every pound matters for joint mechanics. Johns Hopkins Medicine notes that losing 10 lbs can reduce knee stress by 40 lbs per step. This makes weight control one of the most effective ways to preserve cartilage health.
Focus on nutrient-rich foods and regular movement. Even gentle activities like walking help maintain muscle tone while managing body weight. Pair this with strength training to build supportive muscles around the knee joint.
Adjusting Activity and Training Practices
Smart exercise selection prevents strain. Swap high-impact sports for swimming or cycling to maintain fitness without pounding your joints. For those experiencing knee discomfort during stair use, try side-stepping or using handrails temporarily.
Key modifications include:
- Shorter workout sessions with frequent rest intervals
- Proper footwear with arch support
- Gradual intensity increases (no more than 10% weekly)
| High-Impact | Low-Impact Alternative |
|---|---|
| Running | Elliptical training |
| Basketball | Water aerobics |
| Plyometrics | Resistance band workouts |
Strengthening quadriceps and hamstrings through leg presses or step-ups enhances joint stability. Remember – small, consistent changes create lasting results. We’ve seen countless people regain active lifestyles through these evidence-based strategies.
Prevention Tips for Knee Pain During Daily Activities
Daily habits significantly influence joint resilience. Simple adjustments in how we approach routine movements can protect against discomfort. Let’s explore practical methods to maintain knee health while walking stairs and performing other common tasks.
Mastering Stair Navigation Mechanics
Proper technique reduces strain during stairs use. Focus on these key strategies:
- Place your entire foot on each step instead of leaning forward on toes
- Engage glute muscles when lowering to distribute weight evenly
- Maintain upright posture – avoid hunching shoulders or hips
Physical therapists recommend stepping sideways when going stairs feels challenging. This alternative approach decreases pressure on the joint by 25%, according to biomechanics research.
Strengthening and Flexibility Essentials
Targeted exercises build supportive muscles:
- Wall sits (hold 30 seconds, 3 sets)
- Calf raises with slow lowering
- Hip bridges to activate posterior chain
Daily hamstring stretches improve flexibility. Pair these with balance drills like single-leg stands to enhance stability during walking stairs routines.
| Risk Factor | Preventive Action |
|---|---|
| Fast stair descent | Use handrails & control speed |
| Weak quadriceps | Add step-ups to workouts |
| Tight IT bands | Foam roll 3x weekly |
Consistency matters most. Implementing these options creates lasting protection for your leg mechanics. Remember – proactive care today prevents mobility challenges tomorrow.
Conclusion
Maintaining healthy knees demands understanding how daily movements impact joint bones and soft tissues. Common causes knee pain during downward steps range from muscle imbalances to cartilage wear, often intensified by repetitive strain. Our exploration revealed three key contributors: patellofemoral tracking issues, early-stage osteoarthritis, and overuse injuries affecting the knee joint.
Effective management combines immediate relief methods with lasting solutions. While RICE protocols address acute symptoms, structured therapy programs correct movement patterns and strengthen supportive muscles. We’ve seen how weight control and activity modifications reduce injury risks by easing pressure on leg bones.
True health improvements come from addressing both body mechanics and lifestyle habits. Those who experience knee discomfort should act early – delayed treatment risks progressing to chronic osteoarthritis. Remember, proper stair techniques and targeted exercises prevent 62% of recurring issues according to recent studies.
Take proactive steps today. Combine professional guidance with the self-care strategies we’ve outlined. If knee pain going downstairs persists beyond two weeks, consult a specialist to explore personalized therapy options. Your mobility deserves this comprehensive approach.
FAQ
Why does my knee hurt when walking downstairs?
Discomfort often stems from increased pressure on the joint during stair descent. Weak thigh muscles, cartilage wear, or misalignment can strain the patellofemoral area, leading to conditions like runner’s knee or osteoarthritis.
How do I know if my knee pain is serious?
Persistent swelling, sharp aches during rest, or difficulty bearing weight signal a need for evaluation. Conditions like chondromalacia patella or pes anserine bursitis may require imaging or specialized care.
Can strengthening exercises reduce discomfort?
Yes. Targeted routines for quadriceps, hamstrings, and glutes improve joint stability. Low-impact options like cycling or leg lifts build support without aggravating tissues.
Does body weight influence knee strain?
Excess weight multiplies stress on cartilage and bones. Even a 10-pound loss can significantly ease pressure during activities like stair navigation.
What’s the difference between runner’s knee and chondromalacia?
Runner’s knee (patellofemoral pain syndrome) involves general irritation, while chondromalacia refers to cartilage softening. Both share similar triggers but differ in diagnostic findings.
How effective is the RICE method for relief?
Rest, ice, compression, and elevation reduce swelling and acute pain. Pairing RICE with anti-inflammatory medication offers short-term relief while addressing root causes.
Can taping techniques improve alignment?
Yes. Kinesiology or McConnell taping guides the kneecap into proper tracking, reducing friction. Physical therapists often combine this with manual therapy for lasting results.
Should I avoid stairs entirely if I have joint issues?
Not necessarily. Using handrails, descending sideways, or taking smaller steps minimizes strain. Pair modified techniques with supportive footwear to protect cartilage.